In the fight against terrorism, one weapon is invisible to the naked eye.
The expertise and materials rogue nations or groups need to design disease-spreading bacteria that could inflict devastating harm on military personnel and civilians are readily available.
So, the U.S. government has recruited an elite team of University of Florida Health researchers and their private-industry collaborators for a crucial mission: to develop a new antibiotic to counter these deadly pathogens.
Like so many technologies developed for the military, a new antibiotic would also be a vital tool in civilian healthcare, where antibiotic-resistant bacteria are constantly chipping away at the effectiveness of current medications.
While the need is urgent, the pipeline for new antibiotics remains just a trickle. For a host of reasons, few pharmaceutical companies are interested in antibiotic development. So when the federal Defense Threat Reduction Agency (DTRA) began hunting earlier this decade for a team to do just that, UF’s Institute for Therapeutic Innovation was among a short list of candidates.
In early 2021, a group of UF Health researchers accepted the challenge. For two years, they have worked with a Salt Lake City biotechnology company, painstakingly sifting through 43 potential compounds.
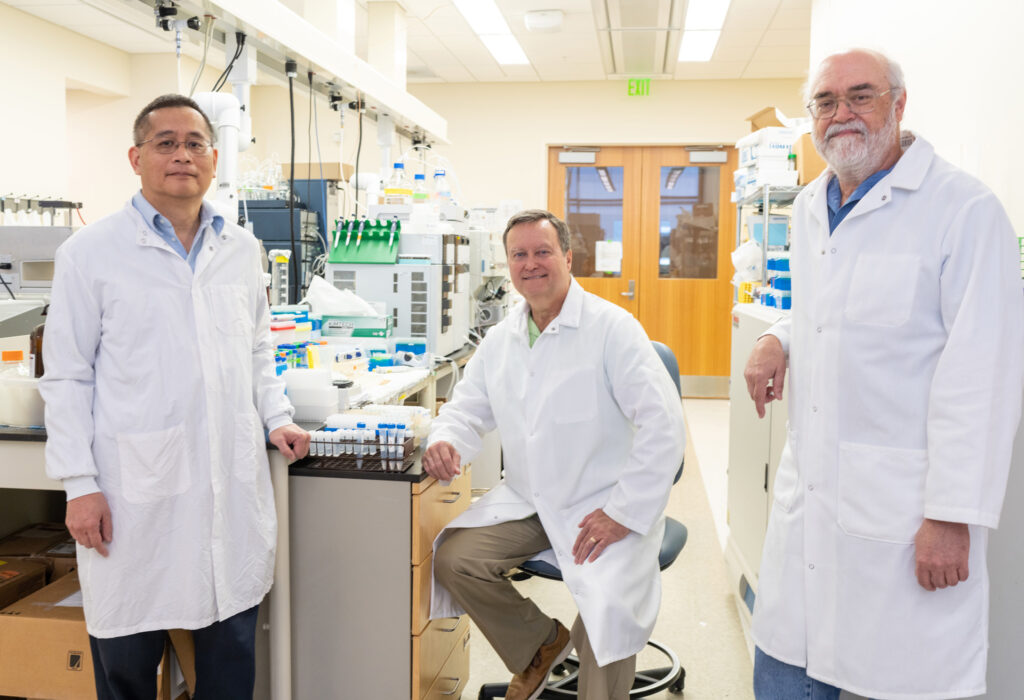
Each member of the UF team brings unique skills to the effort. Henry S. Heine is an associate professor and research microbiologist specializing in advanced antibiotic therapies for biodefense purposes. Bret K. Purcell, a research associate professor, has expertise in applied therapeutics for emerging pathogens. Arnold Louie, a professor and researcher, has expertise in advanced antibiotic therapies for conventional and emerging bacterial pathogens. He is the lead researcher for in vitro hollow-fiber experiments. George L. Drusano, a professor and the institute’s director, uses complex mathematical models to optimize drug treatment and reduce drug-development risks and poor therapeutic outcomes.
and Academic Center at Lake Nona.
A series of experiments in late 2022 produced their first breakthrough with a primary drug candidate and a promising backup. To be effective, a dose of antibiotic compound has to hit a crucial sweet spot: enough to be effective but not enough to be toxic.
Initial testing in small-animal models left the researchers “surprised and excited,” Heine says. Their preferred antibiotic candidate showed effectiveness at lower doses than the scientists expected.
“Now, we’re getting into the nitty-gritty work to verify that there’s no toxicity to be concerned about. And then also to determine: Does it really work? What kind of doses do we need to make it effective?” Heine says.
Agents of Concern
Developing a new antibiotic requires patience and persistence. DTRA gave researchers at UF and Curza, the Utah biotechnology company, $75 million and up to nine years to create a new therapy. Their goal is to develop a drug to destroy bacteria that would otherwise evade current antibiotics. As one of a few universities in the country with the specialized research equipment and experienced scientists needed to create new antibiotics, UF is uniquely equipped to address the challenge, Heine says.
Among the reasons that new antibiotics are relatively rare is that developing and getting regulatory approval can take 10 to 15 years and cost $1 billion or more. With new classes of antibiotics, the failure rate in preclinical development is twice that of other types of drugs. And while development costs are high, the drugs need to be used sparingly to limit the development of antibiotic resistance. All of that makes private pharmaceutical companies reluctant to invest in new antibiotics.
Discovering a novel antibiotic could serve two purposes by protecting U.S. military troops from an engineered biological agent while also treating stubborn infections among the public or hospitalized patients, Heine says.
The drug being developed will be used to fight gram-negative bacteria such as plague, tularemia and another disease caused by Burkholderia pseudomallei, Drusano says. As a biological agent, minute quantities of tularemia can cause skin ulcers, pneumonia and death. Plague, which is caused by the bacteria Yersinia pestis, is typically spread by an infected flea or a bite from an infected animal but also has potential as a biological agent. Burkholderia bacteria cause melioidosis, which can result in fever, pneumonia and potentially fatal septic shock.
“At the end of the day, these are the agents of concern for our warfighters and for the general public in case of an intentional release of these nasty bugs,” Drusano says.
The main antibiotic candidate being studied is a protein synthesis inhibitor. It interacts with a bacterium’s ribosomes, which contain both RNA and protein. The drug works by blocking the bacterium’s protein synthesis. Its unique binding location on the ribosome also makes it much less susceptible to antibiotic resistance — for now.
“Mother Nature hasn’t figured out any good resistance mechanisms to deal with it yet,” Heine says.
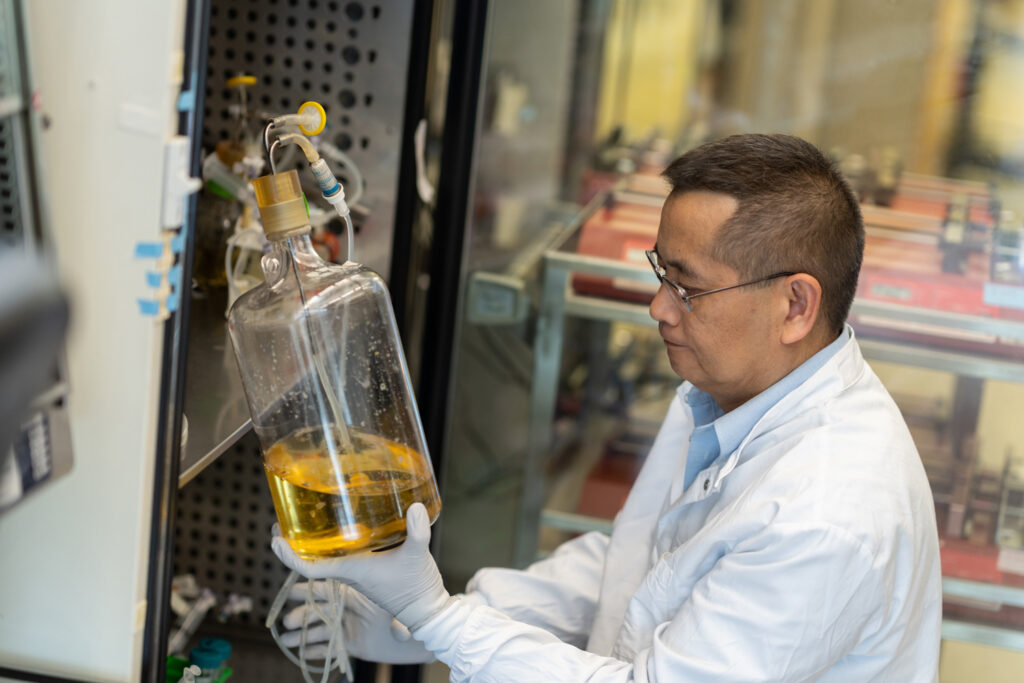
With the support of the federal government, UF and Curza have developed a strong collaboration to develop the new drug. Curza started by making chemical changes to the compounds that are being screened and tested in UF laboratories. Those modifications are crucial to controlling the antibiotic’s toxicity and boosting its potency. That, Heine says, is a key step toward a therapeutic that can someday be used in humans.
Fantastic Four
The four UF colleagues now working on an antibiotic have been collaborators for years, though getting them to UF involved some happenstance. Drusano recruited Heine to a private biomedical research institute in Albany, New York in 2010. Louie had joined the institute at the same time as Drusano. About a year later, while UF was already recruiting Drusano, the New York institute closed. By 2011, they were together again at the UF institute’s labs in Orlando. Purcell joined the group in March 2020, resuming a long collaboration with Heine going back to their days with the U.S. Army’s infectious disease research institute at Fort Detrick, Maryland.
Purcell served nearly 25 years in the Army, listening to recruiting pitches from Drusano and Heine for part of that time.
“I finally got out of the military and decided Florida sounded like a great place to live and work,” Purcell says.
Drusano’s expertise involves complex mathematical models to optimize drug treatment, reduce drug-development risks and lessen poor therapeutic outcomes. In the field of high-consequence bacterial pathogens, Drusano is one of a handful of mathematical experts worldwide. For this project, the UF team through Louie is using a hollow fiber infection model. That technique lets researchers reproduce the ebb and flow of drug concentrations over time in humans or research animals. The model also allows researchers to identify the dose and frequency of an antibiotic that optimizes the killing of a bacterial pathogen while minimizing the probability the microbe may become drug resistant.
“We can actually study how a drug kills the bacterium and also how it prevents or suppresses the emergence of antibiotic resistance. It’s another arrow in the quiver of drug development,” says Drusano, who describes himself as “the one who does the fancy math.”
Antibiotic concentrations fluctuate widely in humans and animals as their bodies metabolize a drug, so trial-and-error testing can be slow and expensive. The mathematical models Drusano has developed allow the team to save considerable time and use far fewer animal models, Heine says. The computer simulations Drusano has helped develop over the years can simulate dosages in 10,000 patients and predict the outcomes in a matter of days.
“George can apply mathematics and modeling to develop doses that we need for effective treatment,” Heine says.
Late last fall, Heine’s team began animal model testing of lead and backup compounds to further assess their toxicity, efficacy and optimal dose against plague bacteria. Proper dosing of any new antibiotic is especially crucial.
“Most of the antibiotics that are available now were developed at least 20 years ago,” Heine says. “That’s why they’re now experiencing antibiotic resistance. No one knew how to dose them properly. The hollow fiber system allows us to do that without using a large number of animals.”
If the compounds continue to show promise and clear all testing protocols, they could gain Food and Drug Administration approval under an agency rule that allows their use in humans after showing safety and efficacy in preclinical models, Heine says.
Heine says the UF team is largely focused on developing an antibiotic that can be used in bioterrorism or germ warfare scenarios, and Curza would likely be called on by the government to produce the new antibiotic for the Strategic National Stockpile, but Curza also may be able to use basic data from the UF collaboration to pursue new therapies for more common infections caused by E. coli or Klebsiella bacteria. The latter can lead to pneumonia or infections of wounds and surgical sites.
The joint effort by UF and Curza is a best-case, mutually beneficial scenario for developing a new antibiotic with strategic defense and potential civilian uses, Heine says. Since UF researchers are focusing their efforts on the antibiotic’s bioterrorism capabilities, important aspects such as toxicity studies and some of the clinical studies are funded by the federal government. That frees up Curza to potentially apply the findings to conventional bacterial diseases with broader civilian applications, according to Heine.
The COVID-19 virus pandemic has also heightened awareness of the deficiencies in the current arsenal of antibacterial drugs, says John W. Kozarich, CEO of Curza.
“We are excited to expand our collaboration with the Institute for Therapeutic Innovation to advance our antibacterial platform to include treatments for biothreat agents in addition to community and hospital associated antibiotic-resistant pathogens. If successful, these unique molecules will represent the first new class of antibiotics discovered in the last 60 years with activity against these pathogens.”
Heine admits that the pursuit of a new antibiotic can be both intense and invigorating. One of those intense moments came last fall as the team awaited important results from some mouse testing. The satisfaction, he says, comes from making progress toward their long-term goal.
“You don’t get a lot of eureka moments in the business but, when you do, they’re extremely satisfying,” says Heine.

and Academic Center at Lake Nona in Orlando.
Photos by Jesse Jones, UF Health
Sources:
George L. Drusano
Professor of Medicine
gdrusano@ufl.edu
Henry S. Heine
Associate Professor of Medicine
henry.heine@medicine.ufl.edu
Arnold Louie
Professor of Molecular Genetics and Microbiology
alouie@ufl.edu
Bret K. Purcell
Research Associate Professor of Medicine
bret.purcell@medicine.ufl.edu
Hear the Story
The audio version of this story is available on our YouTube.


