University of Florida health researchers will use a $11 million, five-year grant from the National Institutes of Health to create a one-of-a-kind center to generate treatments and prevention strategies for one of the most devastating issues critically ill patients face.
 The Sepsis and Critical Illness Research Center, the first in the nation, will study long-term outcomes in patients treated for sepsis in the surgical and trauma intensive care units at UF Health Shands Hospital, to develop clinical solutions for sepsis as well as illnesses that stem from it and their enduring, dismal effects.
The Sepsis and Critical Illness Research Center, the first in the nation, will study long-term outcomes in patients treated for sepsis in the surgical and trauma intensive care units at UF Health Shands Hospital, to develop clinical solutions for sepsis as well as illnesses that stem from it and their enduring, dismal effects.
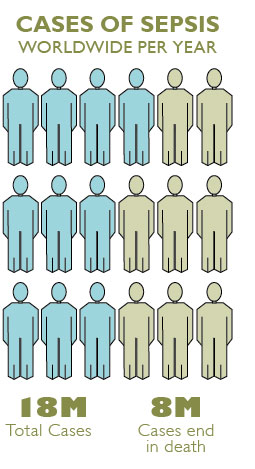
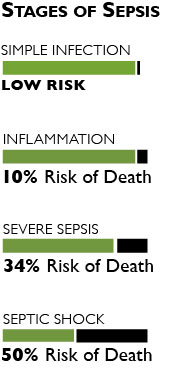
Sepsis is a severe, systemic combination of infection and inflammation that can shut down organs, depress or overactivate the immune system and cause death. Death from sepsis was once common, but improved treatments help many people survive. Severe sepsis leaves lasting effects, however, that scientists are only beginning to understand.
In 2012, after decades of research, UF scientists identified a condition they call persistent inflammation, immunosuppression and catabolism syndrome, or PICS. The syndrome afflicts thousands each year, mostly elderly people who survive sepsis but do not recover fully. PICS will be a focus of the UF Sepsis and Critical Illness Research Center.
“They get sent to long-term acute care facilities and many of them never really ever rehabilitate,” said Frederick A. Moore, head of the new center and chief of acute care surgery at UF Health. “This is increasingly being recognized, and we think we at least have a partial understanding of how this happens. It’s really just a chronic inflammatory disease and people lose a lot of lean body mass. After they lose all their lean body mass, they really can’t get rehabilitated.”
UF Health work on sepsis got another boost with publication of a New England Journal of Medicine article describing similarities between the body’s response to cancer and inflammatory diseases. Lyle Moldawer, professor and vice chair of research in the UF College of Medicine’s department of surgery, and Richard Hotchkiss, professor of anesthesiology, medicine and surgery at Washington University in St. Louis, wrote the article promoting the testing of anti-cancer drugs in inflammatory and immunosuppressive diseases, and the other way around.
 “If these drugs are effective in one of these diseases, they may well be effective in many others. The article is a plea to investigators not to work in silos,” Moldawer said.
“If these drugs are effective in one of these diseases, they may well be effective in many others. The article is a plea to investigators not to work in silos,” Moldawer said.
With the U.S. population age 65 and older expected to reach 92 million by 2060, sepsis and PICS are poised to demand more resources.
Moore will lead one of four main projects in collaboration with the UF Institute on Aging, to examine the course and outcomes of chronic, critical illness that follows sepsis in patients who have been in ICUs and will look at long-term cognitive and physical effects.
This and other projects will draw on a database of information on markers of PICS in patients’ blood, tissue and urine samples, as well as data on patients’ cognitive and physical function.
Mark Segal, associate professor and chief of the UF Department of Medicine’s division of nephrology, hypertension and renal transplantation, and Azra Bihorac, assistant professor of anesthesiology, medicine and surgery in the College of Medicine, will lead a project to study how sepsis affects the kidneys and how these organs may contribute to PICS and other chronic illness.
Moldawer, Philip Efron, assistant professor of surgery and anesthesiology, and Christiaan Leeuwenburgh, professor and chief of the division of biology of aging in the Department of Aging and Geriatric Research, will explore the role of immature immune system cells in the onset of PICS.
The fourth project will focus on the debilitating effects of muscle wasting. A. Daniel Martin, professor in the College of Public Health and Health Professions’ Department of Physical Therapy, will lead the project.
Source:
- Frederick A. Moore, frederick.moore@surgery.ufl.edu

