Azra Bihorac says one of the most important collaborations for doctors and nurses in the future will be with the computer at a patient’s bedside.
Computers will become as important as stethoscopes in hospitals and clinics, says Bihorac, whose research at UF Health focuses on artificial intelligence and emerging technologies for the care of critically ill patients.
“Emerging technologies provide an enormous opportunity for physicians to be able to collect data and process it on the fly in an intelligent way,” says Bihorac, the R. Glenn Davis Chair in Clinical and Translational Medicine. “To process every clinical data value for every patient, for the human brain, that is too much. But using the capacity of AI, we can synthesize the data and come to an intelligent conclusion.”
Computers instructed by precise algorithms will unlock data now buried in electronic health records, report readings from sensors that monitor patients, and record real-time data from more traditional tools like thermometers and stethoscopes and blood pressure cuffs, organizing the data onto a dashboard for everyone on a care team to see.
Technology won’t replace doctors — it’s not a competition between people and machines, Bihorac says — but it will help doctors deliver better care.
And doctors, she says, are ready.

To process every clinical data value for every patient, for the human brain, that is too much. But using the capacity of AI, we can synthesize the data and come to an intelligent conclusion.
– Azra Bihorac
The advent of electronic health records brought the advantage of portability, but also created an avalanche of information nearly impossible to process. Doctors and nurses have long clamored for a way to navigate the labyrinth of data to extract information they need without having to wade through masses of data they don’t need.
“Here’s the data, in these records, but how do you meaningfully use that data?” Bihorac says. “Doctors are looking for that next step.”
That next step is on the way in the form of GatorTron™, a first-of-its-kind technology designed to mine electronic health records in a new way, says William Hogan, the director of biomedical informatics and data science in the UF College of Medicine.
GatorTron™ is a collaboration between UF and NVIDIA, an AI partnership that began with a gift to UF of an NVIDIA DGX SuperPOD AI supercomputer, the nation’s most powerful university-owned artificial intelligence supercomputer. A team of researchers from UF and NVIDIA worked to develop GatorTron™, using 10 years of anonymized medical data from more than 2 million patients and 50 million patient interactions with UF doctors.
By combining forces — research expertise, patient data and computing power — the UF/NVIDIA team came up with a model for GatorTron™ in just seven days.
“What we’ve been able to accomplish with GatorTron™ that’s never been done before is build a model using clinical notes — up to 90 billion words,” says Hogan, one of the leaders of the research effort.
OneFlorida
That big data and health care marry well is no surprise to Betsy Shenkman, who was a big data scientist before the term “big data” was popular.
Early in her career, she mined data from insurance companies to find commonalities in the records that would yield insights for health care. She had mentors who tried to talk her out of this line of research and mentors who encouraged it.
Today, Shenkman oversees really big data. She is the director of the OneFlorida Clinical Research Consortium, a resource with health data for 16 million Floridians, and countless Floridians who have benefitted from OneFlorida research are likely glad she listened to the mentors who encouraged her appetite for data.
Although Shenkman has seen what big data can do, it’s about more than data.
“OneFlorida was not created just for the sake of having data,” says Shenkman, chair of the health outcomes and biomedical informatics department. “OneFlorida really was created to improve the health of Floridians and to contribute to knowledge nationally about how to improve the health of adults and children and older adults throughout the United States.”
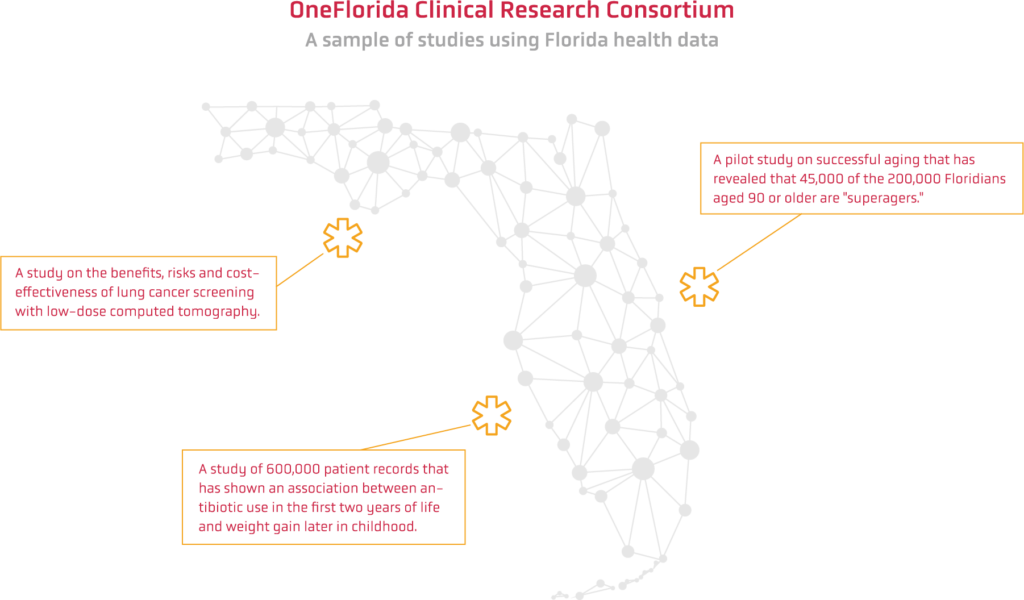
And she’s seen how deploying data for research can pay off. Among the dozens of studies:
- Two UF researchers are using OneFlorida data to evaluate the benefits, risks and cost-effectiveness of lung cancer screening with low-dose computed tomography, particularly the long-term effects of false positive diagnoses, with a $1.4 million grant from the National Cancer Institute.
- A team of UF researchers made up of experts on aging, neurology and the brain, are working on a pilot study on successful aging. What they found in the OneFlorida data surprised them: 45,000 Floridians age 90 and older are “superagers,” meaning they are free of Alzheimer’s, dementia or stroke, and live independently with few hospitalizations or emergency room visits. That is out of a population of more than 200,000 people over 90 in the third most populous state.
- Researchers used 600,000 patient records for a study of antibiotic use in the first two years of life to examine any relationship between antibiotic use and weight gain later in childhood. The study showed an association between the two, adding to the body of evidence that physicians need to be careful about prescribing antibiotics to very young children.
Shenkman says the volume of records helps researchers, but so does the quality of the data. Within the OneFlorida Data Trust is information on diagnoses, medications, procedures and some demographics, all anonymized to protect patient confidentiality. The trust is overseen by the OneFlorida Clinical Research Consortium and the UF Institutional Review Board. Because it represents 4,100 providers across 1,340 practices and 24 hospitals and patients in all 67 counties, the diversity of the records is also a key benefit for researchers.
“Most clinical trials today are conducted with people from predominantly European descent,” Shenkman says. “The beauty of OneFlorida is that because we have such great coverage throughout the state, we have great diversity in terms of the race and ethnicity of the people whose data are in the Data Trust. We have great diversity of age, we have people living in urban areas, rural areas.
“Our goal is to include more diverse populations in our studies, so we have a better understanding of what works for patients who are African American, what works for patients who are Hispanic or Latino,” Shenkman says. “Yes, the data are important. Yes, the computing power is important. But most important is the people and their health.”
From Research to Care
OneFlorida has gathered the data that makes it possible to find the right cohorts for clinical trials and studies, and now GatorTron™ will speed up the process, Hogan says. Before GatorTron™, assembling a group of patients to enroll in trials or studies could take months because of the painstaking effort of extracting the right patients from the database.
GatorTron™ cuts that time frame to minutes.
The natural language processing model developed for GatorTron™ is the first clinical model of its scale in the world. Duane Mitchell, director of the Clinical and Translational Science Institute and assistant vice president for research, says GatorTron™ can read medical language and mine data at a speed humans can’t replicate, and that means faster clinical trials and results.
“One of GatorTron™’s strengths is that it is much more adept and able to read and retrieve medical information with uncommon speed and accuracy,” Mitchell says. “This takes advantage of the computer power and rich medical data that UF has available.”
Organizing data in a way that makes sense for patient care is important, too, Bihorac says.
She and her team in the Precision and Intelligent Medicine Partnership — a multidisciplinary group of researchers in data science, AI and informatics — are looking at ways computers can reduce bias, error and preventable harm in patient care.
Developing tools that can be used in real time is important for patient care, Bihorac says, and one such tool her team has developed is DeepSOFA.
SOFA stands for sequential organ failure assessment, and traditional SOFA yields a mortality prediction score based on the status of six organ systems. DeepSOFA is powered by an algorithm developed by Bihorac’s team and uses deep learning to process data and discover trends in patient conditions.
To evaluate DeepSOFA’s accuracy, the team analyzed data from more than 85,000 former patients at UF Health and a hospital in Boston. DeepSOFA consistently outperformed SOFA. The traditional SOFA model tended to underestimate the severity of illness and predict relatively low chances of death for both survivors and non-survivors.
DeepSOFA also outperformed the traditional model in a single-patient case, in which a female patient was admitted to a hospital and later died from an obstructed blood supply to a lung. Two days after the patient was admitted, DeepSOFA predicted a 50 to 80 percent probability of death, compared with a 5 percent prediction by the traditional SOFA model.
In the final five hours before death, DeepSOFA estimated a 99.6 percent chance of mortality compared with 51.5 percent for traditional SOFA.
“DeepSOFA provides a quick summary of the risk of complications and why the computer thinks those patients might have complications,” Bihorac says. “It’s a really intelligent snapshot of a patient’s condition.”
It is the first time that deep-learning technology has been used to generate patient viability scores, the researchers said. The next step is to integrate DeepSOFA with electronic health records in real time.
Making Advances with AI
Medicine has a host of intractable problems with solutions that advance incrementally, if at all. Researchers hope AI will provide the fuel for long-sought movement.
To jump-start AI research on all fronts, UF Research provided $1 million in seed funding for new ideas through the Artificial Intelligence Research Catalyst Fund. Among the 133 proposals, 20 were funded, including one on Alzheimer’s disease (AD) research by materials science and engineering Professor Juan Claudio Nino and psychiatry and neuroscience Assistant Professor Marcelo Febo. The two are collaborating on a means of using AI to detect the early onset of AD.
One of the limitations on research in AD is not having the computing power for the machine learning … The computational power we need makes it advantageous to be doing this work at UF.
– Marcelo Febo
AD has been at the center of several decades of focused clinical and genetic research, yet much of the evolution of the disease remains unknown. Nino and Febo are attacking the problem from two fronts. From an engineering viewpoint, Nino is using his expertise in brain-inspired network architecture and connectomics. From the medical side, Febo is deploying 17 years of work in functional MRI and biophysics. Using UF’s boosted computing power, the two will use recent advances in fMRI and image analysis to look for biomarkers for early diagnosis and treatment of AD.
In mouse models, the Nino and Febo labs have recently shown that targeted network attacks on brain connectivity matrices reveal differences between diseased and healthy brains. Expanding the work from mouse models to human models, however, will require supercomputing.
“Machine learning and AI algorithms can reveal patterns that we cannot identify or detect ourselves,” Nino says.
Febo says analyzing the brain as a network and how communication occurs between different regions of the brain requires massive computing power.
“One of the limitations on research in AD is not having the computing power for the machine learning and algorithms we need to apply to three-dimensional images, like fMRI,” Febo says. “The computational power we need makes it advantageous to be doing this work at UF.”


Nino describes the network connectivity evolution using a roadmap as an example. If you wanted to travel from Gainesville to Orlando, there are multiple ways to go, and perhaps I-75 is the best. But if there is an accident on I-75, a motorist might try US 441 instead. The brain, too, will try to connect in different ways when faced with an obstacle due to lesions or degeneration of the neural pathways. Although humans often cannot detect such incremental changes in brain connections and activity, an algorithm can analyze millions of connections and help identify potential biomarkers for disruptions in connectivity associated with the onset of AD.
The AI catalyst grant also will fund work on mathematical models, which Nino and Febo plan to use to attack connections to see how the brain’s network responds. Finding patterns in the relationship of one area of the brain to another will be a key to learning more about — and eventually treating — AD, which is projected to affect more than 100 million people by 2030.
Eye on the Patient
AI can also help in monitoring patients, Bihorac says.
“Quite simply, AI can observe the patient in a way no human can because we don’t have the resources and manpower,” Bihorac says.
In one current project, Bihorac and her collaborators examined patient care in the intensive care unit, where one nurse cares for one patient. That seems like a high level of interaction at first glance, Bihorac says. But when the nursing workflow was examined, it showed that nurses only spent an average of 20 percent of their time with eyes actually on the patient. The other 80 percent was spent charting and in other activities.

“In other words, the patient is not observed 80 percent of time, even in the ICU,” Bihorac says. “Things that are very subtle, like changes in facial expression and body movements associated with pain or agitation, often go undetected.”
Sensors, however, can help. Using sensors placed throughout a hospital room, a patient can be observed more intensively, and sensors can pick up on cues that signal a change in health status more quickly. Sensors can track activity, mobility, fall risk, facial expression and more, and convey the information to doctors and nurses in real time.
Bihorac also sees AI as a means of boosting equity in health care, helping health care environments like smaller hospitals and clinics deliver the same level of care as larger, better-resourced institutions.
“AI can help us level the playing field,” Bihorac says. “Not all physicians have the same training; not all hospitals have the same resources. We can give physicians from all backgrounds the same training and tools, and then it really doesn’t matter if you’re in a small community hospital. AI can level the playing field for patients, no matter where they are.”
A human caregiver with access to accurate, computer-enabled information will make better decisions than a human without access to that information, Bihorac says.
But in any scenario, she says, “the human is the most important element.”
Sources:
Azra Bihorac
R. Glenn Davis Chair in Clinical and Translational Medicine
abihorac@ufl.edu
Betsy Shenkman
Chair of the Health Outcomes and Biomedical Informatics Department
eshenkman@ufl.edu
William Hogan
Director of Biomedical Informatics and Data Science, College of Medicine
hoganwr@ufl.edu
Juan Claudio Nino
Alumni Professor of Materials Science and Engineering
jnino@mse.ufl.edu
Marcelo Febo
Associate Professor and Director of Translational Research Imaging, Departments of Psychiatry and Neuroscience
febo@ufl.edu
Hear the Story
The audio version of this story is available on our YouTube.
Related Websites:
Precision and Intelligent Systems in Medicine Research Partnership