“Do you remember what it was like in March and April when we had to mobilize the intellectual resources of the world?” — UF historian Betty Smocovitis
In 2020, as an uneasy world wrapped its arms around a future of uncertainty and risk, researchers around the globe responded the only way they knew how: an all-hands-on-deck approach to science.
As University of Florida science historian Betty Smocovitis observed the unfolding drama from lockdown in her home, she saw something new.
“What we were watching is what it can look like when a planet literally coordinates its brains, and science is at the heart of it,” says Smocovitis, a professor with a dual appointment in the history and biology departments.
At UF, researchers joined what has been called the pandemic pivot, changing directions from decades-long research programs to apply their skills to what likely will be viewed as the greatest science challenge of a generation.
“All the disciplines were reorienting their expertise, literally turning around and saying, ‘There’s a crisis; what can I do to help?’” says Smocovitis, who began incorporating the spreading pandemic into her own course as early as January. “And it wasn’t just scientists; it was the social sciences, the humanities, the clinicians, the theorists. People were coming from almost every direction.”
In the modern history of science, some events stand out: the Manhattan Project, the polio vaccine, smallpox eradication, and Apollo 13 bringing stranded astronauts home against all odds. The difference with COVID-19, Smocovitis says, is how engaged the public became with science, hungry to learn along with the experts.
“It’s the first time, I think, in the history of science that we saw science on the front page. Not scientists, but actual science, as people grappled with terms like exponential growth and what it means to flatten the curve, how a virus spreads. We’ve never seen anything like it.”
Confronted with problems, scientists responded with “what if …” Ideas big and small emerged as UF researchers—some from makeshift lab benches on kitchen counters—began to tackle any aspect of the pandemic to which they could lend expertise.
When ventilators became a scarce resource, UF designed new models. When testing materials were in short supply, new tests were developed. When N95 masks disappeared from shelves, an abundant surgical cloth was repurposed to protect health care workers. When aerosols became a concern, an international team was assembled to study their behavior. And reams of data, the gold standard for tracking a global health threat, were analyzed in near-record time by UF’s world-class high performance computer, HiPerGator.
By design, the scientific process is not agile. From idea to publication in a journal, the process is meticulous, even plodding in a one step forward, two steps back fashion.
But scientists, it turns out, are agile.
In 2020, confronted with uncertainty and risk, UF scientists responded with ideas and quickly put them to the test. Even as UF’s $900 million research engine came out of lockdown and purred back to life in the summer, COVID work stayed strong, much of it boosted by a special $2 million internal research fund. And, as Smocovitis notes, 2020 will make a mark on research projects for years to come.
But here’s how it all started, a glimpse at how UF’s science team responded with agility and ingenuity to the pandemic.
A Big Need
Samsun Lampotang got an email on March 16 from a colleague who laid a problem on his doorstep. Medical centers were buying ventilators the way the public was buying hand sanitizer and toilet paper, and the supply was drying up just as the need was about to skyrocket.
By April 12, his colleague predicted, there would be a surge of coronavirus hospitalizations and a whopping shortage of nearly 1 million lifesaving ventilators. The government had turned to General Motors and Ford to pick up the slack, but those assembly lines could hardly be retrofitted overnight.
Lampotang, a professor of anesthesiology and a prodigious inventor whose first invention was a ventilator, thought about the shortage for a split second then sent a graduate student to Home Depot for PVC pipe and sprinkler valves.

“I was not daunted by the concept of building a ventilator because this was not my first rodeo,” says Lampotang, who develops simulators that allow medical procedures to be tested on devices before they are used on patients. “I was daunted by the concept of having to supply 950,000 in four weeks. How do you make that happen?”
Using household parts was key, Lampotang says. One country alone purchased 30,000 ventilators in March, drying up not only ventilators but the supply of parts to make them.
“When you order that many, you suck up all the components. It’s like if you’re a baker, and someone ordered a gazillion cakes,” says Lampotang, the director of UF’s Center for Safety, Simulation & Advanced Learning Technologies. “Good luck finding flour, yeast, eggs, to make cakes.”
From retirement, UF associate professor Gordon Gibby pitched in. In addition to being an engineer and a doctor, Gibby is a gifted coder, so he wrote the code and tested the device on his dining room table before posting the code online, open source and free to anyone. The ventilator can be made for $400; the next cheapest version is $10,000.
Lampotang continuously updated specs as he refined the device, and one day, while trying to do an update on the website, he could not log on. He called tech support. The problem? There were 150,000 people on the site checking out the instructions.
The need for ventilators in the U.S. has waned, but in Africa, some countries had no ventilators or just one for two million people. Already, South Africa and Mauritius have built the open source ventilators, and UF’s Center for African Studies has helped with webinars in French and English.
“It all happened so quickly,” Lampotang says. “I was still processing what I’d heard about the coronavirus when I got that email, but there was no way I could stand on the sidelines when I knew I could help.”
Airborne Threat
Bala Balachandar studies complex multiphase turbulent phenomena that can’t be tested in a lab, such as nuclear explosions or volcanic eruptions, and had no notion of diving into coronavirus science until he kept hearing one word more and more often: aerosols.
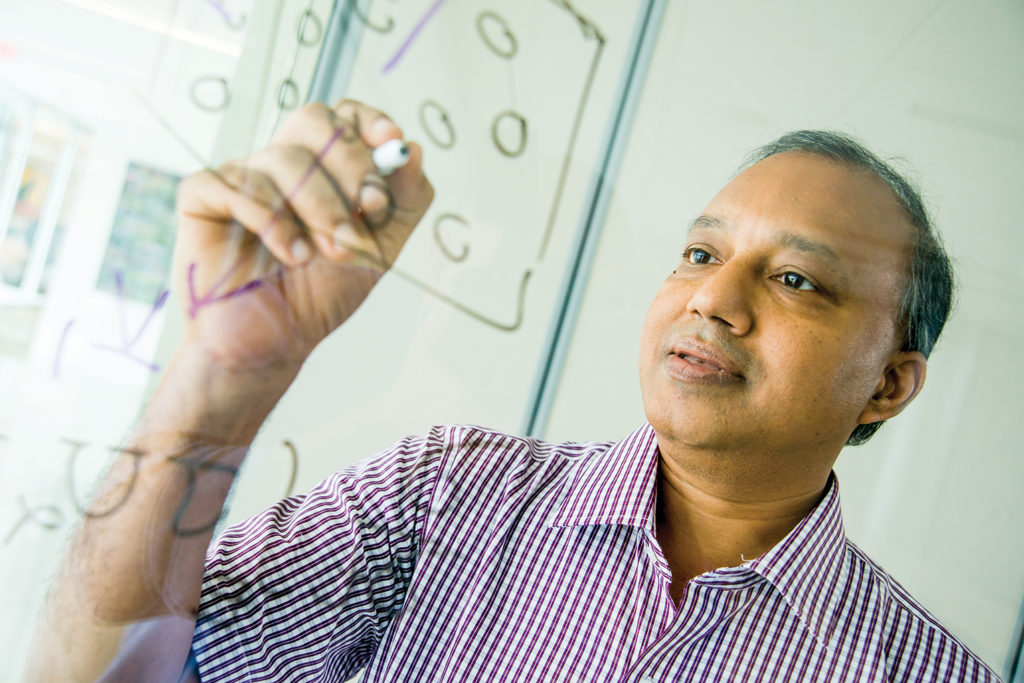
is focused on understanding how aerosols spread the virus.
The unsettled science of how coronavirus infects humans revolves around tiny viral particles that can travel great distances through the air, just the kind of multiphase turbulent flow problem Balachandar tackles in the U.S. Department of Energy-funded Center for Compressible Multiphase Turbulence.
As all the world was going crazy sanitizing surfaces, Balachandar organized an international team, and his lab quickly assembled simulations of how human exhalations travel after a cough, or a sneeze, a laugh, a song, a breath, potentially carrying tiny coronavirus-laden aerosols along with them.
“It is increasingly clear that airborne transmission is an important contributor to rapid spreading of the disease,” says Balachandar, a professor of mechanical and aerospace engineering with funding from the U.S. Navy to study atomization of liquid spray. “We don’t have the fundamental knowledge we need at this moment. Our job is to develop that kind of knowledge.”
In July, 239 scientists asked the World Health Organization to acknowledge airborne transmission’s role in viral spread, and later, the Centers for Disease Control and Prevention did just that.
In August, an interdisciplinary UF team posted results of a spot test in a hospital room with two coronavirus patients. The team isolated live coronavirus in air samples collected about 7 feet and about 16 feet from a patient with an active infection, but not outside the room, thanks to infection control practices.
“The next step is to be able to say how it got there; was it a one-time occurrence?” Balachandar says. “That’s where we come in. We want to show how and why the aerosols can travel that far.”
The theoretical framework is science in motion, as the lab conducts simulation after simulation. Already they know that 6 feet of social distancing is not always enough to keep aerosols at bay and that many variables govern how the coronavirus-laden aerosols waft through the air.
“I first thought that COVID would go away, so I didn’t want to redirect my interest,” Balachandar says. “But then it became very clear COVID isn’t going anywhere.
“This is not a very easy problem to solve,” Balachandar says. “But we need to try. Even if we solve COVID, it’s just a matter of time and a couple of years before something else comes along.”
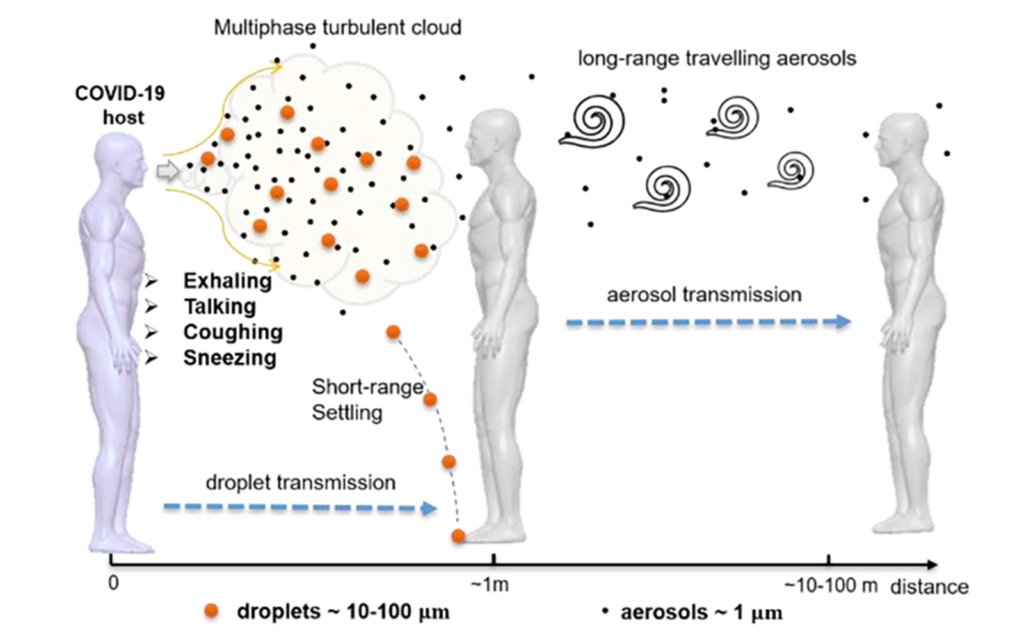
Two Routes of Transmission
Direct Route
- Large drops move ballistically
- They fall rapidly to ground
- Settle on surfaces
- Transmitted by contact
Indirect (airborne) Route
- Smaller drops stay up for a long time
- Carried by the puff
- Dispersed by turbulence
- Inhaled easily and cause infection
Testing Bottleneck
Testing quickly emerged as a key issue in the pandemic. UF researchers sprang into action early, building a lab in 10 days that could test the particularly vulnerable older population of The Villages, a massive retirement community in Sumter County south of Gainesville. And UF engineers teamed up with Exactech, an orthopedic technology firm, to use 3D printers to make nasal swabs when it became clear the swab supply would run low.
Researchers in fields removed from coronavirus also switched directions.
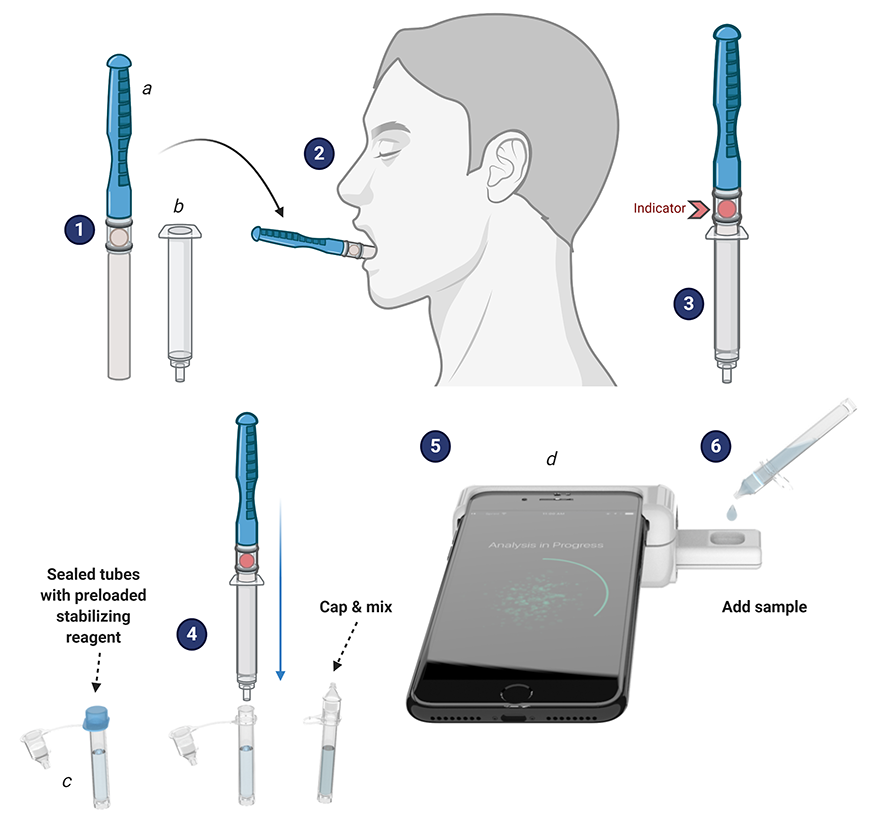
Rhoel Dinglasan, a malaria researcher, retooled a new saliva-based malaria test he developed a year ago. The breakthrough, a game changer for malaria, became a breakthrough for COVID-19 when he discovered it would detect coronavirus.
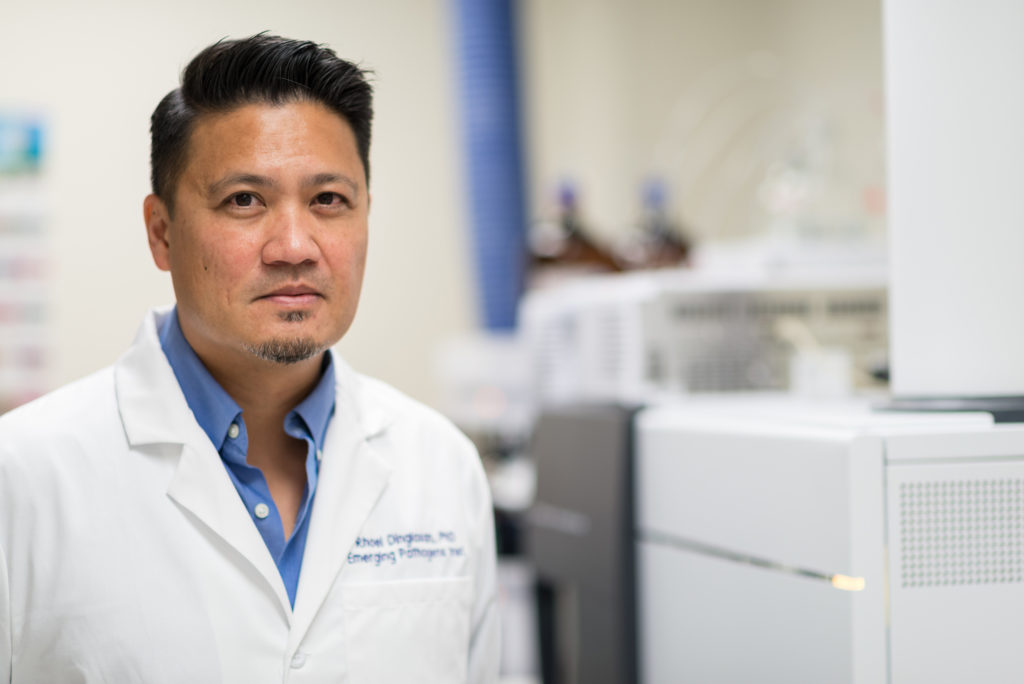
The smartphone-based rapid saliva test Dinglasan and his colleagues developed detects not only malaria and COVID-19, but anemia, too, and won second place in a National Institutes of Health competition along the way. The test utilizes a CLIP-CAM, an adapter attached to a smartphone that allows a detection cassette to be inserted into a slot. The camera flash excites the detection system in the cassette, which can then be read by a smartphone app, with results available in 15 minutes or less—no lab and no health care worker.
“It’s kind of a selfie for your health, isn’t it?” says Dinglasan, a faculty member in the College of Veterinary Medicine and the Emerging Pathogens Institute.
Piyush Jain took another path to developing a home test. The test uses a strip comparable to a pregnancy test.
“The idea is to have a paper-based system where people can just look at it and say, yes, you have it, or not,” says Jain, a chemical engineering professor whose background is in pharmaceutical sciences and biomolecular engineering.
Jain’s lab works on CRISPR-based testing for diseases. Long Nguyen, a doctoral student in Jain’s lab, had used CRISPR to detect prostate cancer, HIV and hepatitis C.
“As soon as the novel coronavirus emerged, I saw an application of this technology and immediately jumped right into it,” Nguyen said. “I was super excited not only that the test worked, but also that it showed significantly higher sensitivity compared to other CRISPR-based detection technologies.”

Jain says the test can aid in early detection for patients with an active infection, which would help people know to self-isolate. Clinical validations are almost completed, and the test will soon go before the Food and Drug Administration. The test is also a semi-finalist in the rapid COVID testing category for the XPRIZE, a competition designed to boost innovation, and the team is one of 11 out of 400 to be funded by USISTEF, the U.S.-India Science and Technology Endowment Fund, for out-of-the-box COVID-19 ideas.
The breakthrough is similar to a test in development in California, but with modifications to the CRISPR system that make the test more sensitive, allowing it to work faster.
“We’re not developing a totally new system,” Jain said. “The best analogy is we’re making a better engine for a car that other people are building. When we have a better engine, we can go faster.”
When word of the breakthrough got out on campus, Jain says he was approached by other scientists with ideas to contribute.
“I’m really proud of UF after seeing this response—not just for me, but for COVID-19 in general,” he said. “It’s wonderful.”
Technology and Ingenuity
In the Warren B. Nelms Institute for the Connected World—part of UF’s Herbert Wertheim College of Engineering—researchers found safety solutions in sensors.

Swarup Bhunia invented the ADAPT smart mask, which can detect particles the size of coronavirus droplets and release a mist that clings to the airborne droplets,
causing them to fall to the ground.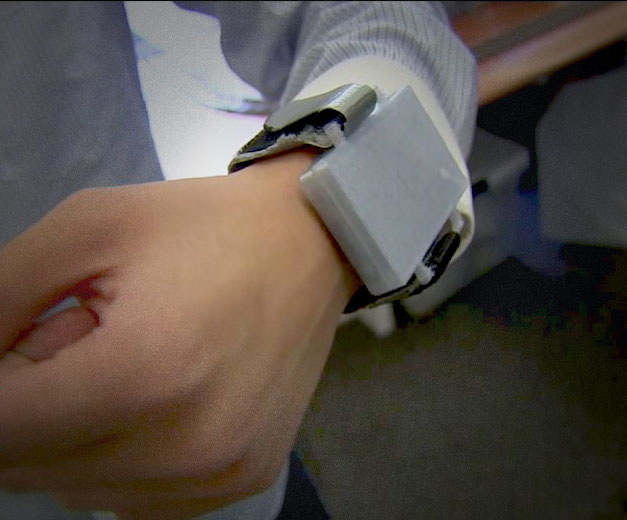
RiskBand is a wearable device that signals students when they are closer than 6 feet to a classmate. The device can also help with contact tracing .
For children returning to school, social distancing is a key to safety, but one with which younger children might struggle. So, researchers developed RiskBand, a wearable device to signal a student when he or she is closer than 6 feet to a classmate. The device can also help with contact tracing because the data can be uploaded at the end of each day and show which students were in close proximity to each other if one turns up sick.
Another wearable, the TRIDENT smart band, continuously monitors a person’s temperature, including subtle changes, so the wearer knows to get a coronavirus test. The devices are in the prototype stage and are being evaluated for accuracy in groups of people. They are designed to be inexpensive—the TRIDENT band’s cost is around $20—and they operate through an app on mobile phones.
Sensors can also be embedded in masks and help clean them and reduce the amount of virus to which the wearer is exposed. Sensors in the ADAPT smart mask, designed by Swarup Bhunia, the Semmoto Endowed Professor and director of the Institute, can detect particles the size of coronavirus droplets and release a mist that clings to the airborne droplets, causing the particles to fall to the ground.
Mask design also got a leg up from nanotechnology. Through a National Science Foundation Rapid Response Research, or RAPID, grant, a team of UF researchers began developing a mask wrapped with nanomaterials—very small synthetic particles—in soap molecules designed to kill the virus after it is filtered by a face mask. That solution became important when health care workers began reusing their masks as shortages loomed.
The interdisciplinary team—combining experts in engineering, nanotechnology, epidemiology, public health practices, virology and infection control—was led by the Department of Environmental and Global Health in UF’s College of Public Health and Health Professions.
One innovative solution for the mask shortage was lower-tech but high-impact.
Hospitals typically discard the fabric used to wrap sterilized surgical instrument trays. But the Halyard H600 two-ply spun polypropylene can block aerosols and droplets, including water, bacteria and other particles.
“This material is otherwise thrown out, so by taking it, cutting it and making masks out of it, we’ve repurposed it,” says Bruce Spiess, a professor of anesthesiology in the UF College of Medicine who came up with the idea.
About 10 masks can be made from one 4-foot-square sheet, and an estimated 500 to 1,000 sheets are available from UF Health hospitals every day, Spiess says. The masks are not intended to replace the gold standard N95—although they passed an N95 test in Australia—but could help fill a need in the face of a critical shortage.
A UF Health team produced kits with precut Halyard material along with ribbons, elastic and nose wires. The kits were distributed around the community, and masks were sewn by a brigade of volunteers. When the masks were returned to UF Health, they were sterilized by ultraviolet light or autoclave before distribution.
“It was meant to be a cottage industry to create a higher-than-surgical mask filtering system that could be made by local sewists when we had no other PPE available,” Spiess says.
Spiess encouraged ingenuity in design, and several prototypes are in development. The mask has gone global, too, with the design being adopted in dozens of countries, such as Hong Kong, India, Germany, Brazil, Africa and on U.S. aircraft carriers.
“I’ve heard from all over the world where these masks have been made,” Spiess says. “Every hospital uses this same material.”
New Directions for Past Research
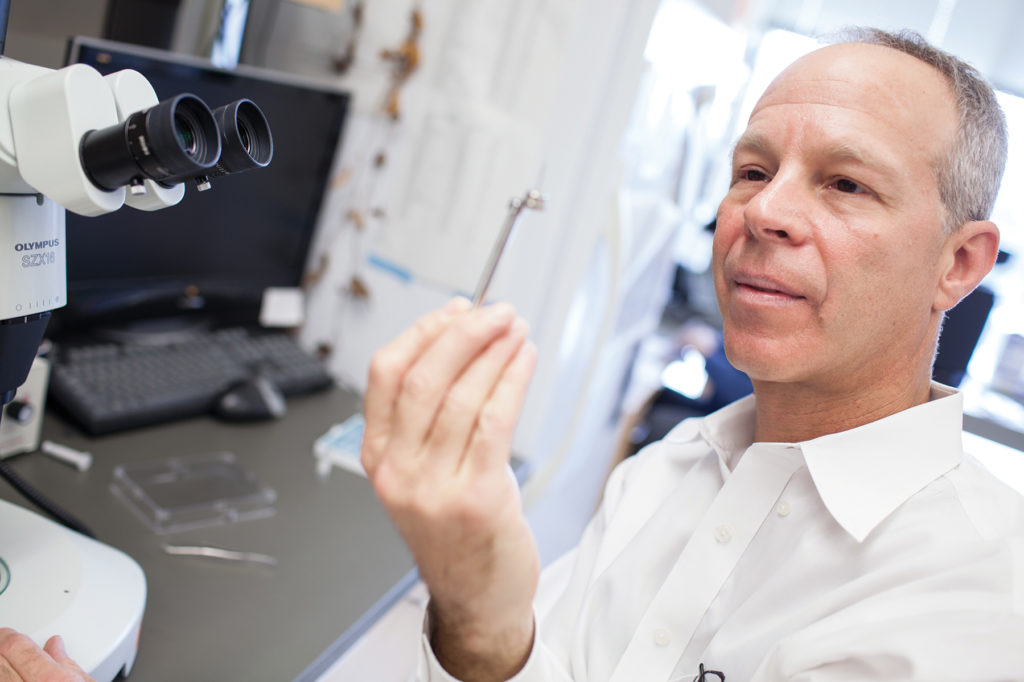
In the quest for treatments for COVID-19, David Ostrov and his colleagues decided to take a shortcut. Bringing a new drug to market can take years, but if they could find a drug already in common use with a long safety record and FDA approval, they figured they could speed up the path to a new treatment.
other viruses, like SARS, will work against COVID-19,
Ostrov had an idea about where to start. He and his colleagues had discovered an inhibitor of ACE2—angiotensin-converting enzyme-2—after the SARS outbreak in 2002. ACE2, at that time only recently discovered, turned out to be the receptor for the SARS virus. The spike protein on the surface of the SARS virus binds to ACE2 on human cells, allowing the virus to waltz in and infect the cell.
Ostrov and his colleagues wanted to know if the ACE2 inhibitor they had discovered might keep the SARS virus from binding to cells, essentially locking the cellular doorway to keep SARS coronavirus out. A collaborator at the National Cancer Institute tested the compound and found that it did, indeed, block SARS, and the work was published in 2004.
“That was part of the trail that led us to where we are today,” says Ostrov, an associate professor in the College of Medicine and the Targeted Therapeutics Program leader at the UF Health Cancer Center.
The first SARS threat passed, but when the new coronavirus, SARS-CoV-2, came along, the older work provided a foundation for new research.
Back in March, Ostrov and his colleagues were asked by a company affiliated with the Global Virus Network to test compounds for ACE2 binding and potential antiviral activity. Those compounds did not pan out, but the researchers went back to their own data from 2011 on the approved drugs they had found that bind ACE2, which is also the receptor for SARS-CoV-2.
The question: Did the approved drugs actually inhibit the coronavirus in the lab? The research team—Ashley Brown, of the UF Institute for Therapeutic Innovation in the College of Medicine; Leah Reznikov, of the College of Veterinary Medicine; and Mike Norris, of the College of Liberal Arts and Sciences—tackled the question with funding from the UF Clinical and Translational Science Institute.

are studying existing drugs that might inhibit COVID-19.
One approved drug that binds ACE2 clearly inhibited the virus that causes COVID-19, their work found. The next question: Would other drugs in the same class also inhibit the coronavirus, perhaps with greater effect?
Ostrov knew he would need more data to answer that question and went “on a worldwide quest” to find it. He found a collaborator at the University of California, San Francisco, and in the health records of more than 219,000 people, the researchers found data both on the patients’ status for infection with SARS-CoV-2 and their drug history for the class of drugs the researchers thought might be beneficial.
“My collaborator was skeptical that this type of analysis could be informative, but went ahead and looked up the statistics,” Ostrov says. “The data we got back were striking.”
In an analysis of common, FDA-approved drugs in the same drug class, three showed a statistically significant association between usage of the drugs and reduced incidence of SARS-CoV-2 positivity. In other words, people in this population who took any of the three drugs were less likely to test positive for SARS-CoV-2.
To find out whether the drugs actually help prevent viral infection and inhibit SARS-CoV-2, Ostrov and his colleagues returned to the lab. They found three approved drugs that inhibit the coronavirus and found that usage of these drugs was associated with lower likelihood of testing positive for SARS-CoV-2.
The drug usage results were parsed by age and gender, and the associations were stronger in people 61 and older, among the most vulnerable to COVID-19, meaning the three approved drugs may have particular benefit in older populations. Randomized placebo-controlled clinical trials will be necessary to determine if usage of any of the three drugs actually prevents COVID.
Ostrov hopes the research provides the basis for an orally deliverable antiviral drug combination, similar to drugs used for HIV and Hepatitis C. The next step, Ostrov says, is publication in a medical journal.
“I’m bursting at the seams, wanting to get this information out there,” Ostrov says.
Viruses, Animals, People
Virologist John Lednicky has been studying viruses, including coronaviruses, for more than 35 years. About four years ago, he developed a test to detect betacoronaviruses, one of four groups of coronaviruses, in Brazilian free-tailed bats, a common bat that is also found in Gainesville.

When coronavirus began making news from China in late 2019, Lednicky pulled out his four-year-old test to take another look. He tweaked it a bit and got it ready for the mass testing in The Villages.
“As soon as China posted the genetic code of this new virus, I was curious to see if my test would pick it up,” says Lednicky, a professor in UF’s College of Public Health and Health Professions. “And I was surprised. My test was a very good fit for the virus. I’m a scientist. We’re always wanting to figure out if our work is helpful for things other than what it was designed for.”
Smocovitis, as a biologist and a historian, was struck by the willingness of scientists in China to share data.
“As a historian of science, it gave me goosebumps,” Smocovitis says. “China uploaded its genomic data and put it on a shared website really early in January. That’s unprecedented.
“They wanted the whole world to work on it. For me, that was a key moment, when this data was literally uploaded and shared with everyone. That is not the Manhattan Project, which was secret, it was not Apollo, which was about winning the Cold War. When you’re looking at something that is this big, there is no one left untouched on the whole planet.”
When the pandemic emerged, Smocovitis was teaching “The History and Evolution of Infectious Disease,” a popular course she has taught since 1997. She was in demand as someone to bring the community at large into the culture of science, writing guest columns and doing a video for the Max Planck Institute for the History of Science and a podcast for the Consortium for the History of Science, Technology and Medicine in Philadelphia.
She noted the zoonotic component, the jump of the virus from bats to people, as a feature in other epidemics and pandemics, and something that had been predicted. Academics, she says, know enough to be scared.
“As a historian, it’s terrifying because I live with the Black Death,” Smocovitis says. “It killed a third of the population of Europe, and when you read the testimonials that speak to you from the past, you really feel that existential threat. These people are dead, and they’re still speaking to you.
“So I don’t think it’s an accident that researchers are dropping what they’re doing,” Smocovitis says. “You take what you know, and you try to make things better.”
Although science has been attacked on occasion, Smocovitis says it is rising to this challenge.
“Is it like the Manhattan Project? No, this is much bigger,” Smocovitis says. “It’s more like an asteroid is coming. How do you coordinate everybody on planet Earth?”
Contributors to this report include Michelle Jaffee, T. DeLene Beeland, Alisson Clark, Leah Buletti, Jill Pease and Sarah Carey.
Editor’s Note: For an archive of more than 100 articles about UF coronavirus research, visit: https://explore.research.ufl.edu/uf-covid-19-research-expertise.html