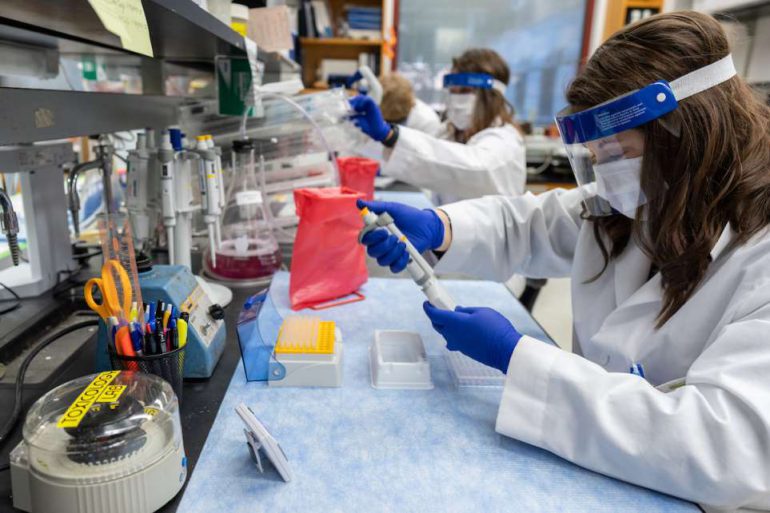
UF Health researchers work to develop COVID-19 vaccine using gene therapy technique.
The technique uses a harmless virus to help fight a harmful virus. In this case, the harmless virus is used to package and deliver a gene from SARS-CoV-2, the strain of coronavirus that causes COVID-19. The gene therapy vaccine can’t replicate on its own but is potent enough to trigger a beneficial, antivirus response from the immune system.

Barry J. Byrne, M.D., Ph.D., a rare-disease researcher and pediatrician, has begun testing two vaccine candidates in animal models. Virology experts at UF’s Emerging Pathogens Institute expect to have initial results soon that will determine if the vaccines effectively trigger virus-neutralizing antibodies against the live SARS2 virus.
The vaccine idea draws on gene therapy techniques developed for other diseases, including causes of debilitating neuromuscular diseases. In those cases, a harmless adeno-associated virus, or AAV, is used to deliver functioning copies of affected genes. Now, Byrne is aiming to use that same delivery vehicle — AAV — to jump-start the process to block the SARS-CoV-2 virus that causes COVID-19 from entering cells.
The approach has some potential advantages over traditional vaccine development, said Byrne, director of the Powell Gene Therapy Center at UF and a pediatrics professor in the UF College of Medicine. Because AAV has been widely studied, researchers likely won’t have to spend as much time establishing its safety given that the effective dose for a vaccine is thousands of times less than in a genetic disease. It also may eventually prove to have a very rapid onset of effect and be more durable than other types of vaccines, especially since the vaccine is only administered once.
Early studies in animals confirm these expectations and the team is ready to assess the effectiveness and toxicology of two closely related vaccine candidates in rodents, which will pave the way for a human study. By August, Byrne hopes to start a 12-month, multi-arm Phase I/II study to assess the vaccines’ single-dose safety and effectiveness in 100 adult volunteers. An emergency use authorization has been requested from the U.S. Food and Drug Administration.
Byrne and his colleagues are also aiming to develop a universal vaccine for future SARS-CoV-2 strains. Multiple mutations — changes in the virus’s genetic sequence — have already been documented by scientists elsewhere. This “genetic drift” underscores the need to develop a vaccine that can be deployed against constantly evolving strains of SARS-CoV-2, Byrne said. To do that, he and Sergei Zolotukhin, Ph.D., also a gene therapy researcher and pediatrics professor, plan to develop a library of various “spike” proteins that the coronavirus uses to invade human cells. Having a catalog of spike proteins is crucial to developing a universal vaccine for current and future SARS-CoV-2 strains, he said. Byrne estimates that developing a universal vaccine would take 18 months.“This is a virus that can change very rapidly. That is concerning because it means any vaccine made today may be ineffective tomorrow.”— Barry J. Byrne, M.D., Ph.D.

“This is a virus that can change very rapidly. That is concerning because it means any vaccine made today may be ineffective tomorrow,” he said.
Initial studies are internally funded and collaboration with pharmaceutical partners is planned for more widespread implementation. Additionally, a request for federal funding is pending.
While there are no licensed vaccines that use AAV, about 25 so-called viral vector vaccines are in various stages of development around the world. Byrne said his approach may have one advantage over some of the others: a shorter, more direct path to clinical use and the significant efforts enable large-scale manufacturing of AAV vectors for other diseases.
At this early stage, Byrne said he hopes that a viral vector vaccine could ultimately be manufactured for only a few dollars per dose. While producing large quantities of AAV is challenging, Byrne notes that biotech and pharmaceutical companies already have some of the needed manufacturing capacity. If an AAV-based vaccine proves to be effective, production could be refocused on the type of virus needed for the SARS-CoV-2 vaccine.
Some two decades ago, Earl and Christy Powell approached UF officials with the idea of starting a gene therapy center. A family friend had been diagnosed with a genetic lung disorder, prompting the Powells to think big about gene therapy research and patient care closer to home. Over the years, the Coral Gables couple’s ongoing support of the Powell Gene Therapy Center has led to significant gene therapy discoveries and attracted world-class scientists. Having that scientific talent and ambition in place is crucial when a fast-moving pandemic such as COVID-19 arises, Christy Powell said.
“It has been very exciting to see what gene therapy has been able to do so far for specific diseases,” she said. “It is just as gratifying to have an opportunity to perhaps make an impact on global health by studying vaccines.”
This story originally appeared on UF Health’s The Post.
Check out more stories about UF research on COVID-19.