Ira Longini has long experience in modeling infectious diseases, from the annual versions of influenza to the exotic chikungunya, and cholera and dengue in between.
“About seven or eight years ago I started working on Ebola — I didn’t publish anything — I just thought it might eventually become a problem, so I pulled together quite a bit of data going back to 1976,” says the University of Florida biostatistician. “I didn’t do much with it because no one else seemed to think it was going to be a big problem.”
When Ebola erupted on the international stage in 2014, Longini was ready.
The disease spread across West Africa in Guinea, Liberia and Sierra Leone. As the epidemic spilled into 2015, it had claimed more victims than all the previous outbreaks combined, and by spring more than 10,000 lives had been lost. The need for rapid assessment of the epidemic turned Longini’s on-again off-again work on Ebola into a 24/7 undertaking.
Today, Longini is on loan to the World Health Organization, which has called all hands on deck for fast-tracked Ebola virus disease vaccine research. Work by Longini and his colleagues is among the earliest research published on modeling the current Ebola epidemic and its spread, and Longini will work at WHO headquarters in Geneva, Switzerland, through the spring, designing vaccine strategies and modeling the efficacy of vaccines when they roll out.
The Centers for Disease Control and Prevention’s early, worst-case estimate — potentially 1.4 million cumulative Ebola cases by January 2015 — treated the region as a “big, random mixing unit,“ Longini says.
He and his colleagues at the Center for Statistics and Quantitative Infectious Diseases, or CSQUID, a joint program of Fred Hutchinson Cancer Research Center in Seattle and UF, decided to design a detailed model focused on Liberia, taking into account geographic and demographic data and accounting for the non-pharmaceutical interventions, such as home health kit distribution and changes in funeral practices.
Prior to the interventions, the research found, 38 percent of infections occurred in hospitals, 31 percent in households, 22 percent in the community, and 9 percent in funerals.
“What you really have are hundreds if not thousands of small epidemics in regions and pockets at high risk,” Longini says. “Our model takes into account that there are many, many epidemic curves.”
The model also predicted the decline in new cases in Liberia, as the interventions took hold. Longini says the model can be useful in designing and analyzing the vaccine trials and, once there is a vaccine or vaccines, the optimal strategies for vaccination, both in the current outbreak and in controlling future outbreaks.
“It’s a mathematical model we can use for the entire region for quite a few other things,” Longini says. “This isn’t over.
“In the reported cases, we just see the tip of the iceberg; we have no idea how many people were infected or what will happen next.”
During his assignment to WHO, Longini will travel to Guinea, where he says outbreaks could be going on that have been missed because of the country’s geography and population distribution. This outbreak’s length, spanning more than a calendar year, also brings up other questions.
“We don’t know yet if Ebola has a seasonal component, if it could come roaring back as we move into spring. We’ve only watched it for one year,” Longini says. “Many diseases, like flu and malaria, have seasonal components, and we don’t know that for Ebola at this point.”
Another difficulty is that the three countries, though neighbors that have been lumped together under the West African umbrella, are geographically and culturally very different.
Sharon Abramowitz, a medical anthropologist who specializes in Liberia, has been trying to explain that, too.
Abramowitz is coordinator of the UF Center for African Studies’ Health in Africa Working Group, an interdisciplinary group of faculty members and graduate students focused on Africa’s huge global burden of disease, from death in childbirth and malnutrition to malaria, AIDS and, in 2014, Ebola.
Early aid workers, Abramowitz says, failed to realize that the scattered rural villages they saw were deeply connected in a vibrant, mobile network that flows back and forth across the borders of the three countries constantly. Unlike in Central Africa, where past outbreaks had been contained in isolated villages, West Africans moved from rural to urban environments and back again in longstanding food, health care, workforce and social networks.
Paul Psychas, a former Peace Corps medical officer and a member of UF’s Emerging Pathogens Institute (EPI), says the three countries’ different histories also complicated matters. Guinea, a former colony of France, speaks French. Sierra Leone, a former British colony, usually turns to the United Kingdom for help, and Liberia, with a long history with the United States, usually relies on the U.S.
Decades of war and corruption in all three countries have made the residents acutely suspicious. Eight health workers were killed in September in a village in Guinea.
“This is where an anthropological understanding of a conflict between humanitarian responders and local populations is really important,” Abramowitz says. “Historically, the government of Guinea has been a violent, corrupt and predatory state, and Guineans have stayed as far out of reach of the state, deep in the forest, as they can. They are very mistrustful of outsiders for very sound reasons.”
In Guinea, international health activities often have occurred in association with the state, making villagers suspicious of aid workers. The removal and quarantine of Ebola patients was consistent with past exposures to state-sponsored violence.
“There is a long history of people being taken away and never coming back,“ Abramowitz says. “Fighting quarantine efforts may seem incomprehensible to us, but to many, this response was rational.”
Abramowitz had been following the work in Guinea of Médecins Sans Frontières (Doctors Without Borders) through news feeds and on Twitter and message boards, but the “uh-oh” moment for her came when the epidemic moved into Liberia. Because of her research on her 2014 book, Searching for Normal in the Wake of the Liberian War, Abramowitz knew the country’s war-ravaged health system had not recovered enough to handle Ebola.
“If Ebola had managed to cross the borders into Sierra Leone and Liberia, it was clear the aid community did not understand the travel patterns and transit routes that connected the three countries. Nearly half of the Liberian population lives along just two or three trunk roads that intersect with the Guinean border,” Abramowitz says. “Once it had crossed into Lofa County, it was a no-brainer that Ebola was going to shoot down to Monrovia (the capital) in a flash.”
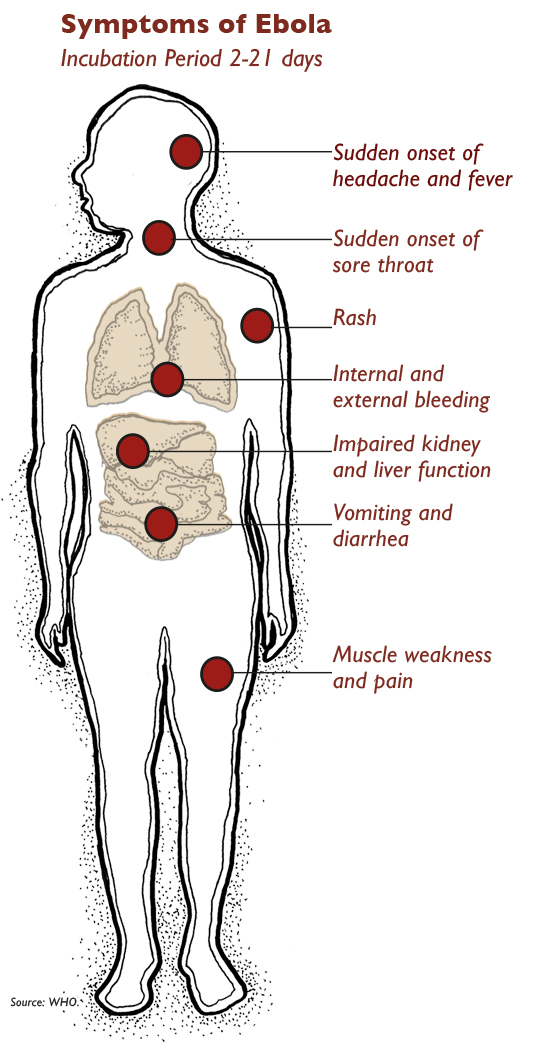
Psychas, a physician, noted that Ebola knocks out a society’s immune system, its health care workers, many dying before Ebola was identified. The three fragile countries averaged one or two doctors per 100,000 population before the epidemic. At one point, 825 health care workers had contracted Ebola and 493 had died. Psychas knew Dr. Sheik Umar Khan, the leading expert on hemorrhagic fevers in Sierra Leone, who died in July.
Psychas also noted that with Ebola taking center stage, people were dying of preventable health issues, like complications in childbirth or infections. Psychas, a malaria specialist, says at one point Ebola was killing 85 people a day in five affected West African countries; malaria was killing 500. He says an international investment in knowledge about pathogens in animals that can spill over into humans is needed. Ebola, and 75 percent of emerging diseases, come from animals.
J. Glenn Morris Jr., the director of UF’s Emerging Pathogens Institute, agrees. Although Americans have been on edge about Ebola, many other diseases — chikungunya, for instance — are bigger threats to the United States.
Morris says Longini’s deployment to WHO is a perfect way for UF to contribute, since EPI cannot work with the Ebola pathogen itself. EPI labs are biosafety level three and Ebola is a biosafety four microorganism. UF often is called upon for mathematical modeling, however, “so on the modeling side we have a great deal to contribute.”
For academic researchers, responding to the Ebola crisis has been problematic, says Sarah McKune, an assistant professor of epidemiology in UF’s College of Public Health and Health Professions.
Research takes a back seat to the need for humanitarian aid. Still, Abramowtiz and McKune were eager to help when a colleague at the World Health Organization in Liberia asked for assistance bringing international attention to data collected in Liberia as the epidemic was peaking from July through October. Abramowitz hoped a rapid analysis of the data and widespread circulation of the findings could help inform the aid response.

Abramowitz, who had been invited to speak on Ebola in Washington, D.C. and other locations nationally, asked her Global Health Cultures class if anyone wanted to help with Ebola research. Thirty students lined up and formed the nucleus of the Ebola Research Group.
With the army of assistants, the data were quickly mined, and Abramowitz and McKune say the results debunked the common image of West Africans as helpless, passive and ignorant.
The data showed several Liberian communities demonstrated rapid social learning, assimilating the information they needed to know and discarding the irrelevant, urban myths that were circulating.
It was the first study of the rate at which social learning around health issues takes place in a public health emergency, using data provided by Liberian health teams.
The data also showed the resilience of the communities when the health care system collapsed with Ebola Treatment Units unstaffed, hotlines unanswered and no help to be found. With survival at stake, families separated the sick from the well and changed their funeral customs.
“Communities will do the unthinkable, the uncultural, in moments of crisis when the future depends on it,” Abramowitz says. “Culture has the capacity to accommodate emergencies by deferring or changing ordinary routines. You didn’t see that portrayed a lot.”
McKune says simplistic messages — wash your hands, avoid sick people — had long since been assimilated, and people were hungry for, and able to use, more complex instructions.
“The assumption is that these populations are unable to understand uncertainty, and that underestimates them,“ McKune says. “In my research on climate change and household food security, we see farmers do it all the time with weather information. We can give people complex health messages, and they will be absorbed.”
Early on, Liberian health officials and the World Health Organization reported that the epidemic was heavily “gendered,” with women making up about 75 percent of the deaths. Traditionally, women are more likely to be on the front line in health care clinics and in preparing bodies for burial, two key risk factors. They also are more likely to be the caregivers for ill family members, making them more likely to come into contact with infectious bodily fluids.
“There were real instances of women knowing in advance they were sacrificing themselves to care for their families,” McKune says.

Psychas, who witnessed a smaller outbreak in Gabon in 2002, says Ebola inspires fear and magical thinking. In Gabon, a local mayor got on the radio to announce that vampires caused Ebola, and other leaders saw quarantines as a way of keeping people from voting in elections. He points out that the U.S. has not been immune to the epidemic of fear: A school in Ohio closed because a school worker traveled on a plane — not even the same flight — as a person who had Ebola.
“In a setting of fear and panic, do we believe in science or do we believe in vampires?“ Psychas asks. “After four decades of experience with Ebola, we know that the biomedical features of this outbreak are the same; it’s the geographic and social context that are different.”
The international response, too, was lacking. After the earthquake in Haiti in 2010, about 800 NGOs showed up to help the country recover, a reaction not seen in the Ebola epidemic, Psychas says.
Longini’s research has shown that travel restrictions were not warranted, and McKune, who travels widely for her research on climate and nutrition, agrees. In June, she traveled to Senegal, her 11-month-old child in tow, for fieldwork. She decided against taking her son to Mali in August, but traveled again in January to Nepal and will be in Senegal and Mali again this summer.
“As Americans, we are a significant driver of global travel, and borders are gone,” McKune says.
Abramowitz has spoken extensively about the epidemic and found her article, “Ten Things Anthropologists Can Do To Fight the West African Ebola Epidemic,” widely circulated on the Internet. One of the early successes of the anthropological response to the Ebola epidemic, she says, was in offering guidelines to humanitarians regarding the management of the bodies of the dead, which prompted conflict with local populations.
She says she would like to see the U.S. response ramped up. Since 2003, in Liberia, the U.S. has spent approximately $180 million a year on health aid. That pales next to estimates that it will cost $6 billion to $10 billion to end the current epidemic, she says. And everyone, she says, should have an international health ID card so that all aspects of healthcare can be linked to a broader system of public health surveillance.
“This is a place where, when people die, it doesn’t really count,“ Abramowitz says. “Does it count if you don’t count them? Every death should count.”

The expedited vaccine trials will attract a lot of interest, not only centered on their success or failure but because it is science at warp speed.
“It usually takes five or 10 years for a vaccine to go through phase one and two testing and phase three trials and licensure, and that big long process is being compressed into six months. It’s an open question: will they work, will they harm people?” says Longini.
Two vaccines are ready for testing, one using a harmless chimpanzee adenovirus and one using a bovine virus to carry Ebola genetic material to trigger an immune response.
Developing the vaccine is only the first hurdle. A vaccination program will be daunting in the chaotic conditions in West Africa, and it is up to Longini and his colleagues to develop vaccination strategies and evaluate them. Three strategies are under consideration.
One, the gold standard for science, is a randomized, controlled trial, in which one group is vaccinated, while another is not to serve as a control. While that would provide the best data, it also raises an ethical issue: Is it OK to give a potentially lifesaving vaccine to some but not others, and how do you choose who gets it?
A second strategy would be vaccinating groups in sequence, with the later groups serving as the control for the first groups. All groups would eventually be vaccinated. Considering that doses may be limited initially, this strategy could work from a practical perspective.
A third strategy is ring vaccination, which vaccinates the family and social circle around an infected individual to halt the spread of the disease.
Longini says it may be possible to use all three and says a vaccine may be the best hope for an end to the epidemic. His previous research has shown that vaccinating 60 percent of a population ends up protecting nearly 100 percent by offering “herd“ immunity.
The trials would not be easy under normal circumstances, Longini says, and they will be even more complicated in West Africa.
“This speed is unprecedented,” Longini says. “It’s a bit of gamble, and there are a lot of question marks. But think what a good vaccine could do.”
Sources:
- Ira Longini, Professor of Biostatistics
- Sharon Abramowitz, Assistant Professor of Anthropology
Related Website:
This article was originally featured in the Spring 2015 issue of Explore Magazine.