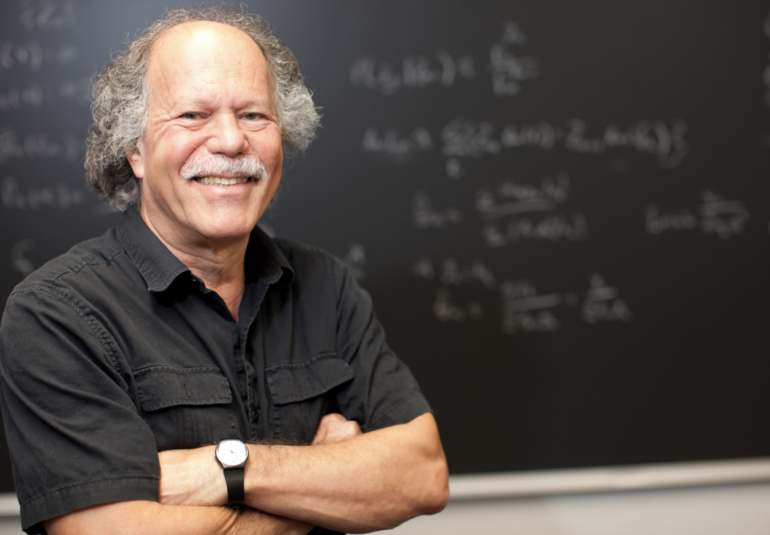
UF researcher Ira Longini works to understand infectious diseases and their transmission dynamics across the globe — and how to halt or slow them down. From dengue in the Yucatan Peninsula to Ebola in the Democratic Republic of the Congo, his work uses mathematical and statistical theory to model infectious disease outbreaks, and how public health strategies or therapeutic interventions can bring them to heel. This year, he’s trained his sights on COVID-19.
Longini is a biostatistics professor in UF’s College of Public Health and Health Professions and UF’s College of Medicine Department of Biostatistics. He is also a faculty member in UF’s Emerging Pathogens Institute and serves as an advisor to both the World Health Organization and the US Centers for Disease Control and Prevention.
Longini’s research contributes to the design of clinical and vaccine trials to ensure they are robust enough to deliver an optimal vaccine or therapeutic agent that is both safe and effective. He also helps devise strategies for the best way to deploy vaccines in different regions of the world.
Working with the WHO
Longini’s experience in helping to design trials and deployment strategies for both dengue and Ebola vaccines positioned him well to assist in the Solidarity Trial organized by the WHO to strengthen the process of testing COVID-19 vaccines. The Solidarity Trial is testing many different vaccine candidates, and placebos, on large numbers of participants in many different parts of the world to search for vaccines that are at least 50% effective.
“I’m working on all aspects of it through my WHO assignment,” Longini says. “We recently published a paper in The Lancet that went into all the concepts behind the COVID vaccine trials including the Solidarity trials. I spent a lot of time at the WHO doing this.”
Longini has worked with the WHO for the past six years. One of his big success stories was the design and analysis of a ring vaccination strategy to contain and eliminate Ebola in Guinea and other parts of Africa. This unique strategy encircles the outbreak with a ring of vaccinated individuals, snuffing the virus out by denying it people susceptible to infection or transmission.
“The vaccine we tested was found to be highly effective,” Longini says. “And that was the only trial effort that found a vaccine. After that, the WHO wanted a whole program to replicate that on a scale for all the major emerging pathogens, not just Ebola. The result is the WHO R&D Blueprint for epidemic threats.”
He helped put together an infrastructure for the blueprint, so that when big outbreaks started occurring, they could assess and find vaccines, therapeutics and control strategies that would pass approval by the necessary regulatory bodies.
Modeling COVID-19
When COVID-19 first emerged, Longini worked with a team of researchers that published a paper in Science on the effect of travel bans on curtailing the pandemic’s spread. They found that locking down the Chinese city of Wuhan had only a modest effect of delaying the overall progression of the epidemic by 3 to 5 days in mainland China, but that it had a more noticeable effect on the international scale by reducing cases up to 80% until mid-February.
He also was a co-author on a commentary recently in The Lancet, that sketched out crucial criteria that should be evaluated in COVID-19 vaccine trials. In this work, the researchers warn that deploying a vaccine with a low efficacy rate may worsen the pandemic if vaccinated people perceive that they are immune and curtail behaviors such as wearing a face mask or social distancing.
Longini has also contributed to an ongoing effort by the Gleam Project to model the pandemic’s trajectory in the US. The projections can be sorted to scrutinize state-level data and they post frequently-updated projections for the numbers of deaths expected on a three- to four-week horizon.
“A lot of reporters call to talk about these models,” Longini says.
He frequently collaborates with other UF researchers, including biostatisticians Natalie Dean and Yang Yang (College of Public Health and Health Professions and UF’s College of Medicine department of biostatistics), and biological disease modeler Thomas Hladish (College of Liberal Arts and Sciences department of biology); all three are also affiliated with the EPI.
Eyes to the future
Longini views COVID-19 as the most recent development in a long pattern of events where viruses in animals have “spilled over” into humans, or what scientists’ term zoonotic spillover events.
“There is no doubt that deforestation and opening up parts of the world that were isolated before is allowing more of these zoonotic spillover events,” Longini says. “And of course, you combine that with our global transportation network, and you get the potential for these large pandemics.”
Through his position at the WHO, Longini works on a list of nine priority diseases that are mostly due to viral spillovers from animal sources. These include the novel coronavirus, dengue, Ebola, Lassa fever, others, and even one that he and his colleagues mysteriously refer to as disease X.
“It’s the next spillover that we anticipate,” Longini says.
In other words, even when COVID-19 is brought to a manageable state, there are other diseases potentially on the horizon, potentially with the ability to create epidemics or pandemics. One of the most important of these is pandemic influenza, a problem that Longini has worked on for the last 45 years.
Creating readiness to monitor and control for future novel diseases is why the EPI supports interdisciplinary teams of researchers, where a biostatistician such as Longini can collaborate with public health and infectious disease experts across the University of Florida — and the globe.
This story originally appeared on UF Emerging Pathogens Institute.
Check out more stories about UF research on COVID-19.