The age-old idiom “finding a needle in a haystack” pales in comparison with finding a virus in the air. At least you can see a needle. Breakthrough work by UF professors Chang-Yu Wu and John Lednicky recently made international headlines when they successfully collected viable novel corona viruses — those capable of infecting people — from air in a hospital room occupied by a patient ill with COVID-19.
Genetic testing matched the SARS-CoV-2 virus they found in the air with virus obtained from the patient. Further testing failed to find the virus in the hospital’s hallways, common areas or waiting rooms; this indicated that the hospital’s infection-control protocols worked as planned. Hospital administrators viewed the follow-up results as a confidence-booster that the testing was accurate and also as a source of comfort about the ambient air quality.
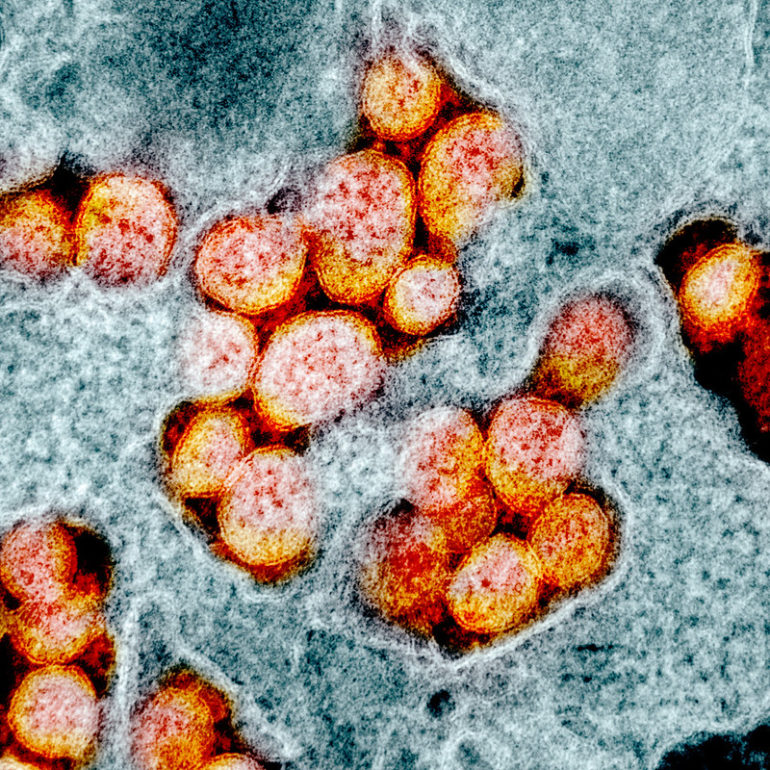
Finding the virus at all was a remarkable feat in large part because it’s so technically challenging to collect viable viruses from air. But it didn’t happen by accident. Wu and Lednicky’s work, which is published on the MedRxiv pre-print server and awaiting journal acceptance, followed a decade of interdisciplinary collaboration between the engineer and virologist who were laser-focused on improving air sampling methods to conserve viruses — which are fragile, protein-coated bits of DNA or RNA — at the point of collection.
When someone coughs, sneezes, talks, shouts or sings, they emit different kinds of respiratory droplets. Some are large enough to fall to the ground, while others are small enough that they float as aerosols. These droplets are often rich in bacteria, fungi or viruses.

Large respiratory droplets tend to fall downward after being coughed, sneezed or exhaled while smaller droplets may float in the air. Image courtesy of John Lednicky and Chang-Yu Wu.
It’s the aerosols that intrigued Lednicky, who is a virologist in the department of environmental and global health at the UF College of Public Health and Health Professions. Could virus-laden aerosols cause infections in people? If they could, what were the public health implications?
Beginning around 2002, Lednicky began using conventional air samplers to search for airborne viruses. But the samplers tended to damage the viruses. In fact, the sampling process was so inhospitable to viruses that while he could often find viral genomic material — which proved only that pieces of viruses float around — it was harder to capture an intact viable virus, one that was whole and infective.
Lednicky wasn’t alone: The challenges and lack of findings were similar for others trying to test air for viruses.
Did this lack of evidence mean that infectious viruses aren’t present in air? Or did problems inherent to the conventional sampling methods prevent researchers from finding them?
The uncertain reliability of collection methods made it hard to know what’s really floating around. And not knowing that made it hard to know whether the transmission of highly infectious respiratory illnesses, such as seasonal flu, were driven more by direct contact via large respiratory droplets or airborne routes via aerosolized droplets.
While most public health experts interpreted the lack of evidence for large amounts of viable viruses in air to mean that there just weren’t a bunch floating around, Lednicky’s instinct led him in a different direction.
Looking for aerial viruses
“The air we breathe is full of viral particles,” Lednicky says. “Bacterial viruses, plant viruses, fungal viruses, you name it. But we only worry about those that can cause infections in humans, the ones that result in disease. Those are the ones we are trying to find.”
More specifically, he trained his sights on infective aerosolized viruses — or those that ride upon the tiny unseen respiratory droplets light enough to waft around in air currents and stay aloft for hours. Conventional wisdom holds that few viruses can remain viable for long in aerosols before they dry out and become inactivated. Therefore, airborne transmission is a dead end. Lednicky was unconvinced.
He was deeply interested in viruses that become suspended in the air column as aerosols, riding tiny particles that measure roughly five to 20 nanometers. But to study these potentially infectious specks, he first needed a reliable method to collect them. Unfortunately, he suspected most air samplers at that time smashed viruses to bits or dried them out and rendered them uninfectious during the collection process. While these samplers could find parts of viruses, or uninfectious virus, they didn’t fully answer his questions about whether active, infectious, intact viruses could stay aloft in aerosols.
In 2010, Lednicky was experimenting with a standard air sampler when — disappointed with its poor ability to collect airborne viruses — he began tweaking it to lower the airflow in ways that countered the manufacturer’s guidelines. Curious to know if others were trouble-shooting the same issue, he turned to Google and the first search result to pop up was a scientific poster about the exact same problem by someone named Chang-Yu Wu.
Lednicky looked him up. Out of all the aerovirology researchers in the entire world, Wu was just a few buildings over in UF’s Herbert Wertheim College of Engineering.
Partnering on particles
Wu had also long puzzled over aerovirology; his interest stretched back to 2006. His lab, located in the department of environmental engineering sciences, was focused upon measuring particles in the air, but to measure them properly in the engineering field, each individual particle must be counted. Wu was also fascinated by aerosolized viruses and he suspected that this was a greater transmission route than was recognized. But to test this idea, he needed to sample viruses from aerosols. He was thrilled when Lednicky reached out.
“It is rare that someone so thoroughly understands and appreciates your research,” Wu says. “Knowing John is the best thing that happened to me during my second 10 years at UF. He changed my life. He was the single person who understood what I was doing. Few people cared about the virus aerosol sampling that I tried to do 10 years ago, but lightning struck when I talked to him.”
Wu’s lab had been studying the problem of how to count aerosolized particles when he was inspired to make the particles larger by condensing water upon them. Bigger particles are easier to count.
Plumping the particles up turned out to be the perfect solution to Lednicky’s problem of capturing viruses from the air. Instead of blowing floating viruses through a collector and slamming them into petri dishes, as conventional samplers dud, Wu’s method of condensing water over the particles and growing them larger, then dripping them into petri dishes, was a nearly perfect solution.
While a single virion may be as small as 20 nanometers, most wild viruses are often bundled with bits of cellular debris, or covered in mucus, salt, or various globs of bodily goo. To ensure they were not missing bits of anything, Wu and Lednicky focused on capturing particles from a few nanometers up to 20 micrometers.
Together, the pair began testing out the best methods for collecting viruses from the air, and then isolating them in a lab — a process that tests whether the collected viruses are capable of entering cells and replicating, which are conditions necessary to cause infection in people.
“I like to joke that virologists have problems that need to be solved,” Lednicky says. “And engineers have solutions in need of a problem. And that’s why our collaboration is so useful.”
A decade together
After working together for a decade, Lednicky and Wu have two pending patents that stem from their 13 co-authored peer-reviewed papers, which focus on improving ways to collect aerial viruses.
Their first major advancement in fine-tuning aerosolized virus sampling methods came when they tested a novel commercially available sampler head-to-head against a conventional type. The novel sampler was based on the same principle that Wu’s lab focuses upon, which is to gently plump each particle up with water as it moves along a moist tube designed on a warming temperature gradient. (Warm air holds more moisture.)
The design is based, in part, upon nature.
“When you inhale, the air moves through your nose past these baffles and into warmer and warmer spaces. Compounded with water vapor in the respiratory system, this action humidifies the air before it hits your lungs,” Lednicky says.
The conventional sampler relied upon forced air to slam particles onto filters on petri dishes or hard surfaces.
Lednicky and Wu used a wild-type H1N1 influenza virus, cultured from the 2009 swine flu pandemic, to create virus-laden aerosols with a nebulizer. Using the wild-type virus was key to rule out any biochemical or biophysical differences between human respiratory viruses and the surrogate viruses often used in sampling studies. Wild type influenza viruses tend to be rod-shaped and up to 1 micrometer in length, they are far longer than the 20 to 300 nanometer, circular viruses that are grown in ideal lab conditions specifically for lab experiments.
The water-based novel sampler collected 74% of the viruses from the air that moved through it, while the conventional sampler collected only 5.6% (plus or minus 3%). It was proof that the moisture method was light years beyond conventional methods. Their results were published in 2016 in the Journal of Aerosol Science & Technology.

This graph shows that the novel sampler captured more infectious particles than the conventional sampler, and that both samplers captured more infectious viruses as they sampled greater volumes of air. Image courtesy of John Lednicky and Chang-Yu Wu.
They have continued to pursue the water-based particle growth method in subsequent studies that plucked all kinds of human flu and cold viruses from the air.
Last April, Wu and Lednicky published a review paper that evaluated various types of air samplers available, and the strengths and weaknesses of each. Despite the many different sampling options, they both agree that the process of condensing water onto the particles works best because it reliably captures the most viable viruses.
“This one has received a lot of attention for a review paper,” Lednicky says. “There’s been a high degree of interest in this paper since the pandemic began.”

A diagram of the water-based growth tube collector, far right, that Wu’s lab has built to condense water directly onto particles in the air that may carry viruses. Image courtesy of John Lednicky and Chang-Yu Wu.
More recently, in a paper published this spring, Wu and Lednicky worked directly with the novel air sampler’s manufacturer to improve its performance. After the COVID-19 pandemic arrived to Florida, they networked connections from the EPI to place the sampler in a student health care center.
They sampled air where people walked and also several meters from main foot-traffic routes. They found evidence of coronavirus OC43, a cause of common colds, and two types of viruses that cause flu.
But they also found the genetic signature of SARS-CoV-2, although attempts to isolate it in a lab were not fruitful. This means that they were unable to determine if the virus found in the air was infectious, or inactive. They inferred that the SARS-CoV-2 virus was aerosolized because it was found in a sample more than 2 meters away from the nearest patient walkways. The work helped to guide mitigation measures, and follow-up air samples found no evidence of the SARS-CoV-2 virus.
They also posited that proactively testing environmental air samples may be more useful for tracking the contagion’s spread than human samples. The work laid the foundation for their latest study that successfully isolated SARS-CoV-2 from aerosols in a patient’s hospital room.
“We are not limited only to medical facilities in our sampling though,” Wu says. “We also work with athletes, fitness centers, restaurants, customer service centers and other groups where there is a concern about transmission.”
Aerosolized virus sampling in the future
“What we’ve shown is that the way you do the air sampling is very important. If you do what everybody else does, you make the same mistakes,” Lednicky says. “Our critics say that if you don’t find anything, then there is nothing in the air. But if you sample differently than everyone else and find something, then they’ll say you contaminated your samples or are doing something wrong.”
The pair have fended off their share of critics over the years, and they recognize that turning the tide on conventional thinking takes time. But they are also driven by the evidence of what they’ve found.
“It’s a matter of understanding the science and the engineering,” Lednicky says. “The engineering is especially important because if you have the tools to test the science, then you have an advantage. That is where Wu’s machine is really the best there is.”
Wu envisions adapting his current sampler design to be lighter weight and more compact for broader applications.
“Right now, it is 40 pounds, and 2 feet by 1 foot by 1 foot. It is really for research purposes,” Wu says. “But nowadays you have these air quality sensors that can plug into your cell phone and you can get the measurements instantly. That is my vision for the future. A low cost, lightweight, virus detector or monitor that could be used by anyone and give real-time results.”
Lednicky hopes that their work will help advance public health interventions not only for the current pandemic but also in terms of how authorities conceive of transmission routes for viral respiratory infections.
Investing in work like this, which bridges disciplines and offers a new perspective for addressing how to study and solve problems involving novel and reemerging diseases, is what makes the EPI unique at the University of Florida.
Check out more stories about UF research on COVID-19.
This story was originally posted on UF Emerging Pathogens Institute.