Combining an anti-inflammatory drug with an antiviral drug reduces recovery time and accelerates improvement for COVID-19 patients, a national study co-authored by UF Health researchers has found.
Patients treated with a combination of the anti-inflammatory drug baricitinib and the antiviral drug remdesivir while they were receiving high-flow oxygen or noninvasive ventilation had a recovery time of 10 days, compared with 18 days for patients in a remdesivir-only control group.
Researchers also found fewer adverse events in patients receiving the combination treatment, and the 28-day mortality was 5.1% in the combination group versus 7.8% in the control group.
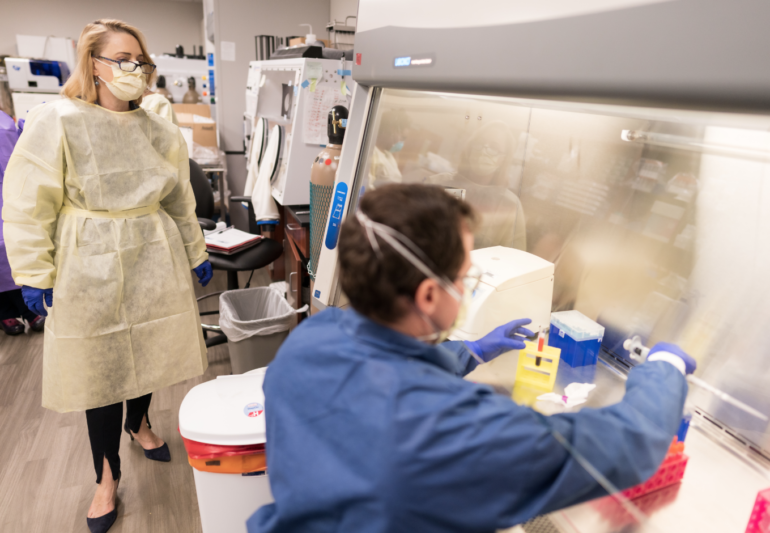
The study, supported by the National Institute of Allergy and Infectious Diseases, was co-authored by Nicole M. Iovine, M.D., Ph.D., UF Health chief epidemiologist, and Marie-Carmelle Elie, M.D., from UF Health’s Department of Emergency Medicine, along with a number of researchers across the country. The study was published in December in The New England Journal of Medicine.
It was the second iteration of a National Institutes of Health, or NIH, study protocol to evaluate therapeutics for those hospitalized with SARS-CoV-2.
The first trial of the study began in May and established remdesivir as a successful treatment for hospitalized adult patients with COVID-19 pneumonia. Remdesivir works against the disease by preventing the virus from multiplying, but substantial morbidity and mortality remained. Emerging data led researchers to hypothesize that the severity of the novel coronavirus may be due, in part, to an abnormal inflammatory response.
“What we’ve learned about COVID this year is that a subpopulation of people infected with the virus had an overly exuberant inflammatory response,” Iovine said. “Exhibiting a response to fight off infection is a good thing, but for some people, it’s way too much. Our goal was to stave off that hyper-inflammatory response triggered by cytokines.”
Enter baricitinib. Baricitinib is commonly used as an anti-inflammatory treatment for those affected by rheumatoid arthritis.
“There was a precedent for trying baricitinib,” Iovine said. “We use powerful anti-inflammatory drugs all the time for a number of other infections. A major theme of adaptive treatment trials is to find useful therapeutic agents quickly. The drugs chosen need to be ones that have already been studied, like remdesivir as a treatment for Ebola. We don’t need to reinvent the wheel.”
Baricitinib blocks the activity of certain proteins and enzymes and interferes with the pathway leading to inflammation.
“Because baricitinib was already in use for rheumatoid arthritis, we knew its safety profile and dosing regimens,” Iovine said. “We know very clearly how it works on a molecular level to reduce inflammatory cytokines associated with severe COVID-19.”
This second iteration of the clinical trial included 30 UF Health patients enrolled by Iovine and Elie. It evaluated more than 1,000 COVID-19 hospitalized adults across the country through 28 days of a double-blind, randomized, placebo-controlled trial in which 515 adults received the baricitinib-remdesivir combination treatment, while 518 received remdesivir and a placebo.
Study results revealed that baricitinib plus remdesivir led to better patient outcomes than remdesivir alone.
Those patients receiving the combination treatment with baricitinib had a median recovery time of one day sooner than those in the control group; recovery in the study was defined as the participant being well enough for discharge, therefore no longer requiring supplemental oxygen or medical care.
More impressively, COVID-19 patients on high-flow oxygen or noninvasive ventilation had a recovery time of 10 days with the combination treatment, compared with 18 days for those receiving remdesivir and a placebo.
Researchers also evaluated patients’ clinical status at day 15 of treatment and found that patients receiving baricitinib with remdesivir had a 30% higher chance of improvement in clinical status, gauged on an ordinal eight-point scale ranging from fully recovered to death.
As positive results of the clinical trials began emerging, on Nov. 19 the U.S. Food and Drug Administration issued an emergency use authorization for baricitinib in combination with remdesivir for adults and pediatric COVID-19 patients 2 years of age and older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
While remdesivir plus baricitinib has shown favorable results, so has another anti-inflammatory drug that is being simultaneously studied and utilized routinely with a similar population of hospitalized COVID-19 patients — the steroid dexamethasone, Iovine said. Dexamethasone is a steroid medication that also modulates the immune system’s response to inflammation.
Thus, the next iteration of the adaptive study will evaluate the results of dexamethasone paired with remdesivir as a COVID-19 treatment, and compare those with results of the remdesivir and baricitinib study.
Iovine and Elie recently enrolled UF Health’s first patient in this trial as research continues to evaluate the best therapeutic treatments for those hospitalized with SARS-CoV-2.
This story originally appeared on UF Health.
Check out stories about UF research on COVID-19.