While many experts are focused on identifying COVID-19 cases and slowing transmission, one UF research team is focused on the pandemic’s fallout on children and households.
In what may be a nationally unique study, researchers affiliated with UF’s College of Public Health and Health Professions, College of Medicine and College of Education are analyzing the social effects of the pandemic on local school-aged children and their families across time, alongside infection rates. The study also digs into connections between beliefs about COVID-19 and actions people take to protect themselves.
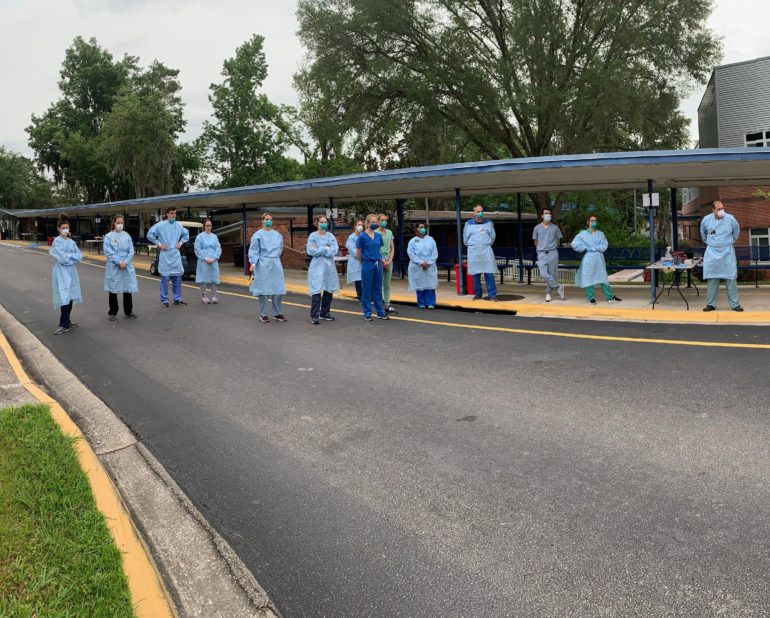
The researchers are six months into a cohort study of students and their family members that tests for active and past infections from SARS-CoV-2, the virus that causes COVID-19.
But in an unusual twist, participants also respond to a questionnaire that seeks to uncover the interplay between people’s knowledge, attitudes and behaviors in response to social changes brought about by the pandemic and linked social and health outcomes in children. The researchers will also examine transmission chains within households, and what role children may play in passing the virus along.
UF Health News previously covered the study’s kickoff at P.K. Yonge Developmental Research School in an article published this past April.
Social insights
Sarah McKune, a research assistant professor in UF’s College of Public Health and Health Professions Department of Environmental and Global Health, uses social science tools to understand public health challenges. Much of her work examines how households manage stress and what makes them resilient to external shocks — such as widespread disease.
“In this study, we are looking at indicators of anxiety, stress, depression and obsessive-compulsive disorder, in both school-aged kids and their household contacts,” McKune says. “We are using questionnaires to examine people’s knowledge, attitudes and practices surrounding COVID-19. The traditional thought is that someone’s knowledge influences their attitudes and behaviors and gives them agency to deal with an issue or a challenge. The way knowledge may change someone’s behavior can either protect them, or make them more vulnerable to the disease.”
Several of McKune’s departmental colleagues are also collaborators on the project: Eric Nelson, M.D., a pediatrician and assistant professor, and UF preeminence professor Tony Maurelli, who is also the department’s associate chair.
“As far as we know, this is the only study of its kind in the country,” says Nelson, who also holds a joint appointment in the UF College of Medicine. “But we feel that a study like this should be done in every state.”
After launching the project in April, participants were retested and offered the survey again in June. Participants will be retested and surveyed again in mid-October, with enrollment of additional participants, and final testing and survey assessment of participants will occur in April 2021. Analysis of the viral and antibody tests is taking place at UF’s Emerging Pathogens Institute.
Seeds of collaboration
Maurelli says the project originated in part from a conversation with McKune.
“Sarah lives across the street from me, and I knew her kids attended P.K. Yonge,” says Maurelli, who is affiliated with UF’s Emerging Pathogens Institute. “We spent an hour and a half talking on my front porch about the school, and the idea of doing this study. I reached out to her because of her specialty in studying social science aspects of public health, and her connection to the school.”
Maurelli then pitched the project to UF’s Emerging Pathogens Institute Director J. Glenn Morris, who facilitated bringing in Nelson, who is also affiliated with the EPI.
“This is the great thing about the eclectic nature of our faculty,” Maurelli says, a microbiologist by training. “It’s a fertile ground for collaborations like this. Which you might never get to do in many other institutions.”
Behavioral links
McKune’s focus on household resilience, coping mechanisms and their impact on overall health, combined with testing the student population for the virus, is unique. Responses from a questionnaire, administered at the same time points as the viral and antibody tests, will be analyzed to understand how the pandemic and parental knowledge, attitudes and practices about COVID-19 may be contributing to, or triggering, anxiety, depression and obsessive-compulsive disorders.
“More than any other outbreak I have ever worked on, COVID sits right at the interface between biology and psychiatry or behavior,” Nelson says. “If you really want to understand transmission, control and mitigation — all of those techniques that you need to be deploying effectively — you have to put both the biology and the behavior in the same research framework together.”
Understanding what people believe about a disease is also helpful for developing targeted public health communications.
“One of the outcomes we are interested in is how can you change public health messaging such that it changes behaviors? How do you get to where people can protect themselves, or strengthen protections at the population level?” McKune says. “If people believe falsehoods about how infections occur, then they have no agency to act to protect themselves. Whereas if they accept facts, backed by science, then they can change their behavior and increase protections for themselves and those around them.”
But how do changed social norms — and new behavioral routines such as wearing masks and washing hands more frequently — affect the mental health of children and their families?
“Sarah has taken it in an exciting direction, which is to look at how one’s anxiety is affected by practices such as good hand hygiene and mask usage,” Nelson says. “How does that interplay between anxiety and actions give feedback to those behaviors? In terms of social distancing, how does that collectively act as a determinant in terms of transmission? It’s a very interconnected triangle between the biology of transmission, the behavior of what people are doing, and then the psychological or psychiatric disorders or disease that come out of it.”
The researchers hope the survey responses will aid understanding as to whether knowledge of the disease, or knowledge of public health guidelines, offers protection against infection.
“Is there a correlation between the depth of understanding of public health guidelines and people’s psychological reactions?” Maurelli says. “In other words, does too much knowledge connect with high or minimal anxiety?”
Understanding how people respond to knowledge about the pandemic may also be helpful in designing public health messages to mitigate anxiety.
“If some kinds of information are having a negative effect, then you can adjust the message, so you get it across without causing people to react in a negative fashion,” Maurelli says. “No one was looking at these issues at the level that we proposed to do it, for the kids and parents who have been left on the sidelines of this pandemic.”
The questionnaire may also help untangle the role of some risk indicators as well.
“We know that race and economics matter in terms of the risk of getting COVID-19 and its associated health outcomes,” McKune says, “What is it about being a person of color that puts you at risk? Is it something that you believe, a shared cultural belief or practice? You begin to see that, sometimes, indicators like race are proxies for a set of norms, beliefs or practices. That’s part of what we are trying to uncover.”
The next survey will also include questions about vaccine hesitancy.
International perspective
McKune, Maurelli and Nelson all have significant experience working internationally and say that in pulling the P.K. Yonge study together over just a few days, they drew upon skills gleaned from work overseas: flexibility, attracting talented colleagues and building contingencies.
The study also uses dried blood test cards, a valuable technique in parts of the world where freezing a blood sample, or keeping it at a stable cold temperature, may not be feasible. The method relies on a simple finger prick to obtain a small amount of blood that can be used for viral or antibody testing.
“We chuckled about doing the testing at P.K. Yonge, because here we are as global health scientists pulling all our tricks out of our hat, to pull off this project in just a few weeks,” Nelson says, reflecting upon this past spring. “It certainly has been an interesting juxtaposition, to apply lessons learned in Haiti or Africa to a problem right here in our backyard.”
But the best part, they all agree, is using their skills to help parents and children in their own communities.
“The faculty and staff at P.K. Yonge, the kids and parents — they were all just so enthusiastic and so cooperative,” Maurelli says. “Sarah, Eric and I really appreciate their participation in this study.”
This story was originally posted on UF Emerging Pathogens Institute.
Check out more stories about UF research on COVID-19.